Session Information
Date: Monday, November 14, 2022
Title: RA – Treatment Poster IV
Session Type: Poster Session D
Session Time: 1:00PM-3:00PM
Background/Purpose: Current NICE guidance for rheumatoid arthritis (RA) states that glucocorticoids may be used for bridging therapy and to rapidly decrease inflammation in acute flares1. However, the recommended route and dose is not specified. Variation has been observed in use of steroids in early RA2. Glucocorticoids are associated with adverse events that can be severe, leading to a strong recommendation by the American College of Rheumatology to avoid long term use3. It is therefore key to assess efficacy of available routes and doses of glucocorticoids to weigh against these risks. We performed a systematic review to assess efficacy of corticosteroids in early RA.
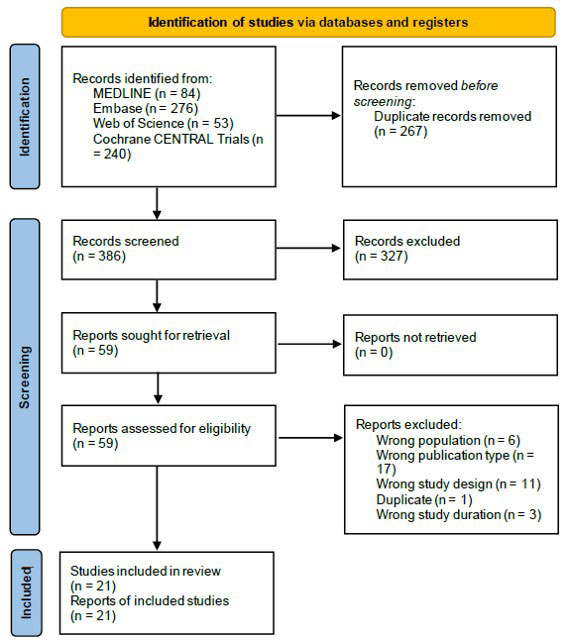
Methods: MEDLINE, Embase, Web of Science and Cochrane Central were searched. Papers included were full text, English language, randomised controlled trials that fulfilled the PICO criteria. The population was defined as adults with early RA with onset < 2 years, the intervention corticosteroids of any route or dose, the comparator conventional DMARDs or placebo, and the primary outcome remission. Functional improvement and X ray progression were considered as secondary outcomes. Screening of results and extracted data was carried out by both reviewers using Rayyan. During data extraction, outcomes were rounded to timepoints of 3, 6 and 12 months, and steroid doses were stratified into low (up to 10mg/day prednisolone or equivalent), medium (15-30mg) and high ( >30mg). Meta-analyses were carried out in RevMan 5.4 when 3 or more studies measured the same outcome at the same dose and route. Quality was assessed using the CASP checklist.
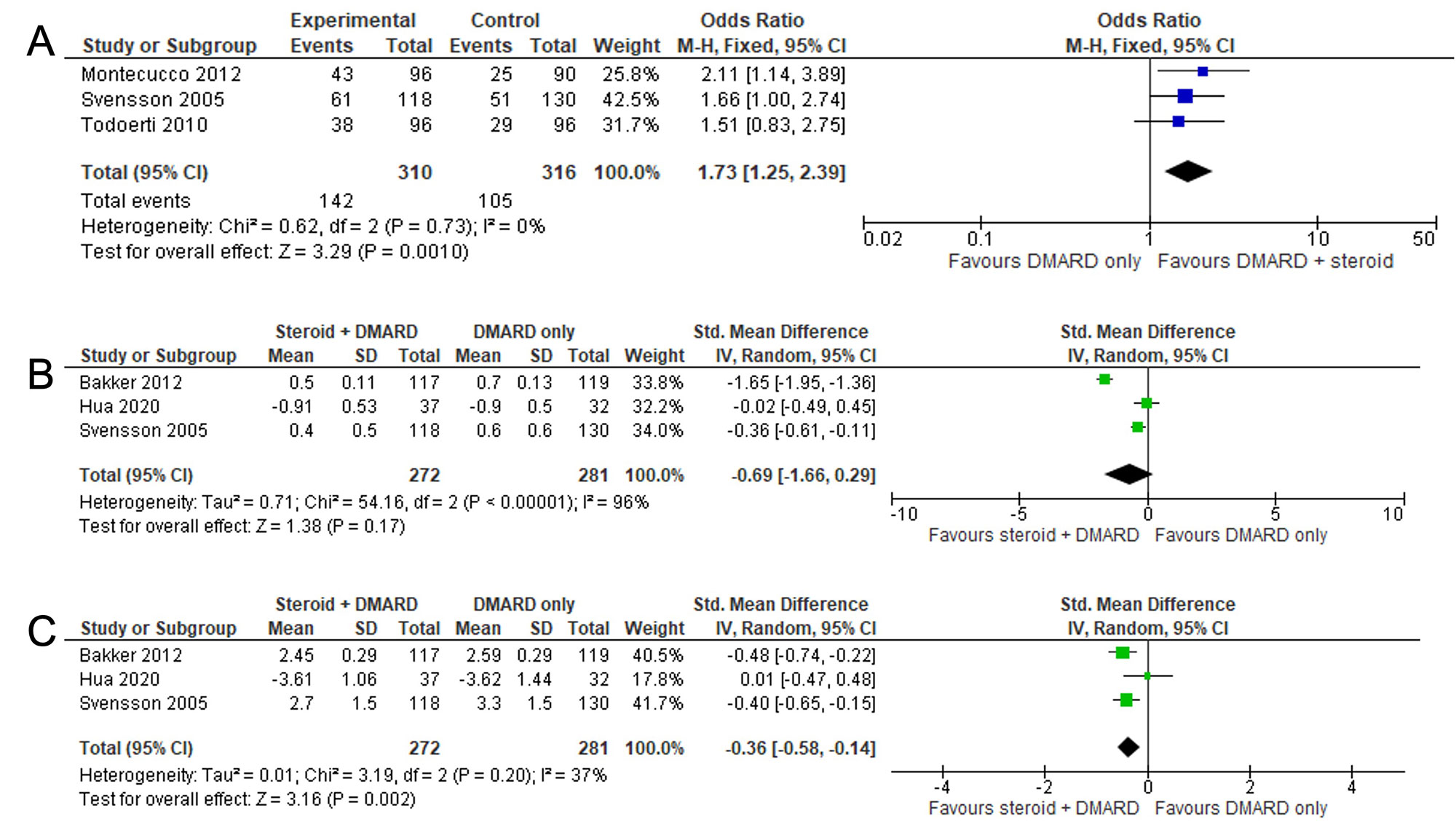
Results: 286 records were available for screening, of which 21 met all inclusion criteria. Three papers measured DAS28 remission rate at 1 year, comparing DMARDs only to DMARDs plus low dose oral steroids (Figure 2A). Low dose steroids + DMARDs were superior to DMARDs alone with odds ratio (OR) of 1.73 (95% CI 1.25, 2.39) with a number needed to treat of 7.9.
Meta-analyses were also possible for HAQ at 1 year (Fig 2B), and mean DAS28 at 1 year (Fig 2C), comparing DMARDs alone to DMARDs plus low dose steroids. Both analyses suggested a potential benefit of steroids; for HAQ scores the standardised mean difference (SMD) was -0.69 (95% CI -1.66, 0.29), and for DAS28 the SMD was -0.36 (95% CI -0.58, -0.15). There was insufficient data to allow meta-analyses at earlier timepoints.
Limited data were available for imaging outcomes at 6-12 months, or comparison between doses and routes and meta-analysis could not be performed. Meta-analyses were not possible for adverse effects; individual studies did not state obvious differences between treatment groups.
Conclusion: At 1 year, DAS28 remission is more likely if low dose steroids are used. Due to a lack of available data, non-oral routes/higher doses and X ray progression could not be analysed. Studies were not designed to detect differences in adverse events. This highlights the need for further clinical research into steroid efficacy in early RA.
References:
1. NICE Rheumatoid arthritis in adults: management. https://www.nice.org.uk/guidance/ng100/chapter/Recommendations
2. Yates et al Rheumatology 2020;59:2035-42
3. Fraenkel et al Arthritis Care & Research 2021;73:924-39
To cite this abstract in AMA style:
Parker L, Gullick N. Which Route and Dose of Corticosteroids Is Most Effective in Inducing Remission in Early Rheumatoid Arthritis? A Systematic Literature Review and Meta-analysis [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/which-route-and-dose-of-corticosteroids-is-most-effective-in-inducing-remission-in-early-rheumatoid-arthritis-a-systematic-literature-review-and-meta-analysis/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/which-route-and-dose-of-corticosteroids-is-most-effective-in-inducing-remission-in-early-rheumatoid-arthritis-a-systematic-literature-review-and-meta-analysis/