Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: RA treatment involves an iterative approach to identifying effective medications for patients. While response varies, there is little in-depth understanding of patients’ perspectives of their experiences when not responding to treatment and consequences on HRQOL. This mixed methods study addresses this gap, investigating patient perspectives on the experience of non-response and the relation with HRQOL.
Methods: This phased study was conducted in collaboration with the Arthritis Foundation, their INSIGHTS initiative (Schifferdecker et al., 2020), and members of their RA working group.
Phase 1 included semi-structured interviews with adults with RA (N=15) to understand the non-response experience and inform survey development. Transcripts were analyzed using a mixed inductive and deductive approach.
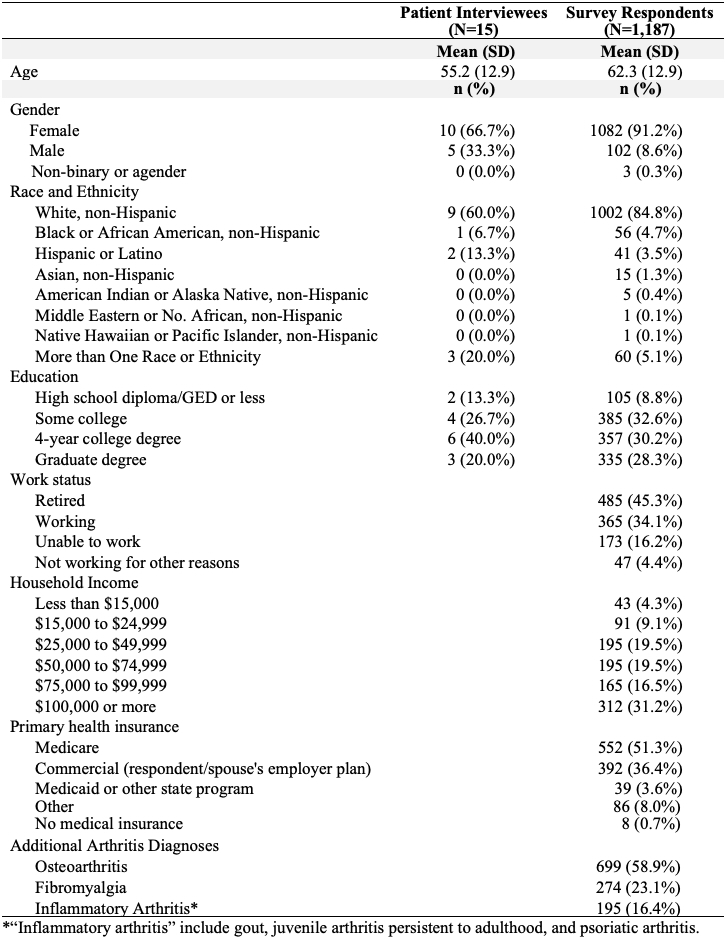
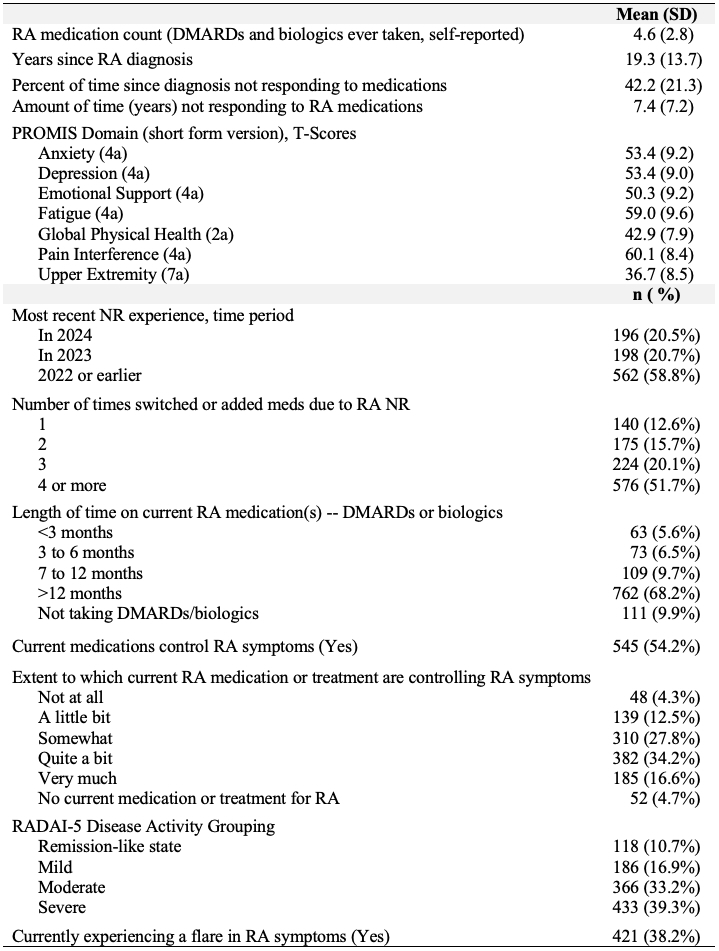
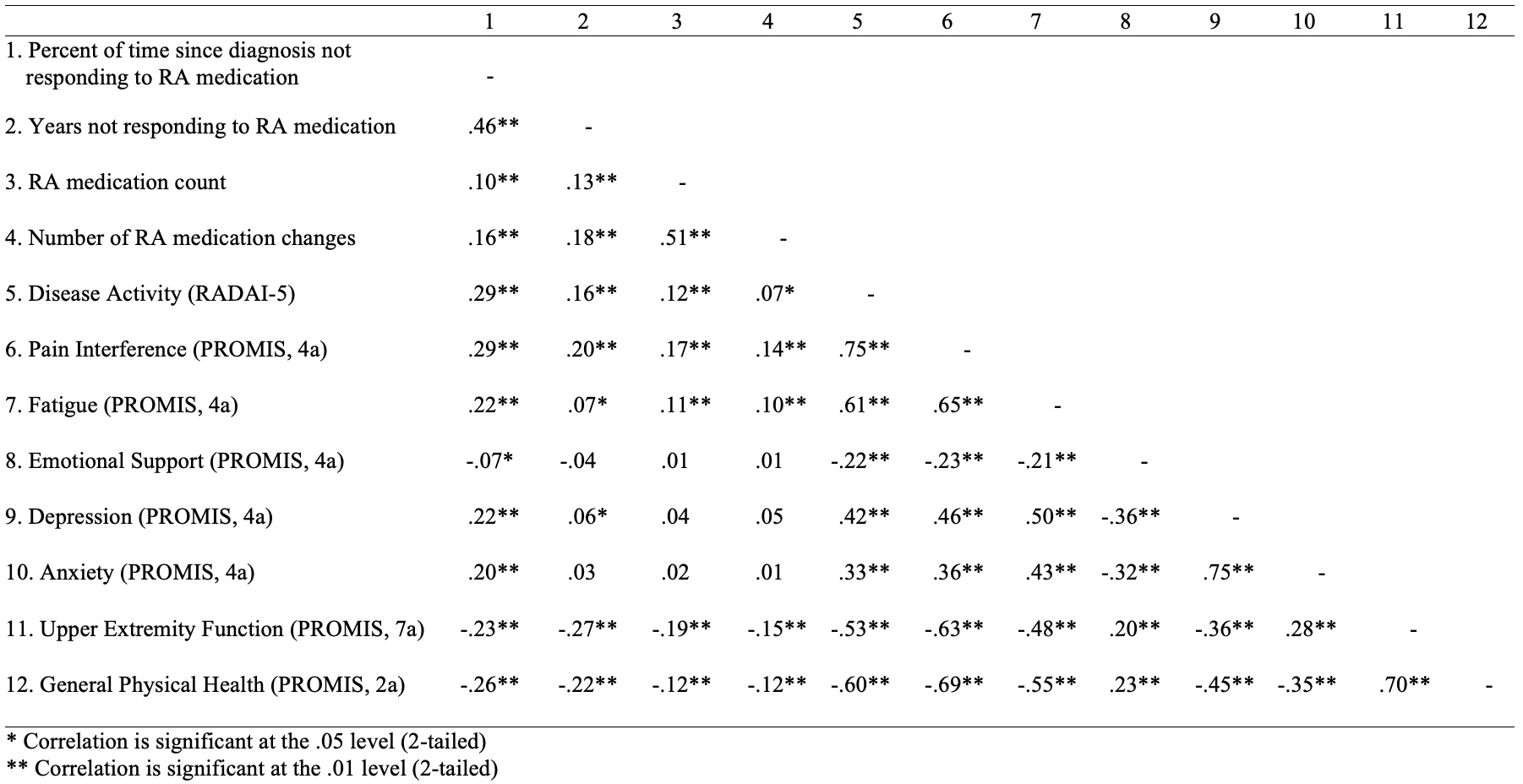
In Phase 2, we created a 113-item survey which included several PROMIS® short forms reflecting HRQOL and researcher-generated items based on the qualitative results to assess non-response experience. We emailed the survey to 9,093 participants in the INSIGHTS study who indicated an RA diagnosis. While clinical data confirming ACR criteria for RA were not available, with advice from rheumatologists we deemed participants eligible if they had taken 1 or more qualifying DMARDs or biologics and were diagnosed by a physician. Eligible participants experienced 1 or more of these medications not controlling their RA symptoms. Descriptive statistics (Tables 1-2) and Pearson’s correlations (Table 3) were calculated. Structural equation modeling is planned.
Results: Interviews: Interviewees described negative impacts of non-response on their mood and functioning, frustration and apprehension trying new medications, and the “devastating” experience of having a medication work initially and later fail. They often described the importance of patient-doctor relationships and not being “brushed off.” HRQOL outcomes (e.g., activities of daily living, reduction in pain) were most important for participants.
Survey: From March-May 2024, 1,748 individuals responded to the survey. For the 1,187 eligible respondents, 97.7% received their RA diagnosis from a rheumatologist, the average time since diagnosis was 19.3 years (SD=13.7), and 41.2% had a recent non-response experience. Compared to the general population PROMIS T-score mean of 50 (SD=10), participants in this study had worse mean T-scores for upper extremity function of 36.7 (8.5), pain interference of 60.1 (8.4), fatigue of 59.0 (9.6), and both anxiety and depression of 53.4 (9.2 and 9.0, respectively) (Table 2).
The percent of time not responding to RA medication had small but significant (p< .001) associations with disease activity (r(1097)=.29), pain interference (r(1093)=.29), general physical health (r(1082)=-.26), fatigue (r(1095)=.22), depression (r(1089)=.22), anxiety (r(1084)=.20) and upper extremity function (r(1087)=-.23; Table 3).
Conclusion: Interviewees described the onerous process of pursuing treatment that repeatedly failed to improve their RA symptoms and the importance of shared decision-making. They described significant impacts of non-response on HRQOL outcomes, which is supported by our survey findings.
To cite this abstract in AMA style:
Carluzzo K, Knight E, May S, Bernstein L, Mueller K, Bingham C, Schifferdecker K. When Medications Fail: A Mixed Methods Study Evaluating the Experience and Health-Related Quality of Life (HRQOL) of Adults with Rheumatoid Arthritis Non-Responsive to Treatment [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/when-medications-fail-a-mixed-methods-study-evaluating-the-experience-and-health-related-quality-of-life-hrqol-of-adults-with-rheumatoid-arthritis-non-responsive-to-treatment/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/when-medications-fail-a-mixed-methods-study-evaluating-the-experience-and-health-related-quality-of-life-hrqol-of-adults-with-rheumatoid-arthritis-non-responsive-to-treatment/