Session Information
Session Type: Poster Session A
Session Time: 8:30AM-10:30AM
Background/Purpose: Identifying knees at risk of worsening osteoarthritis (OA) could help to identify individuals in need of interventions. While gait and physical activity are considered important for knee OA pathogenesis, the interrelations between these factors are complex and challenging to specify using traditional statistical models. Machine learning approaches remove the need to pre-specify these underlying relationships among factors when predicting an outcome. Our objective was to investigate the ability of gait and physical activity measures to predict medial tibiofemoral cartilage worsening over 2-years in the Multicenter Osteoarthritis Study (MOST) using machine learning.
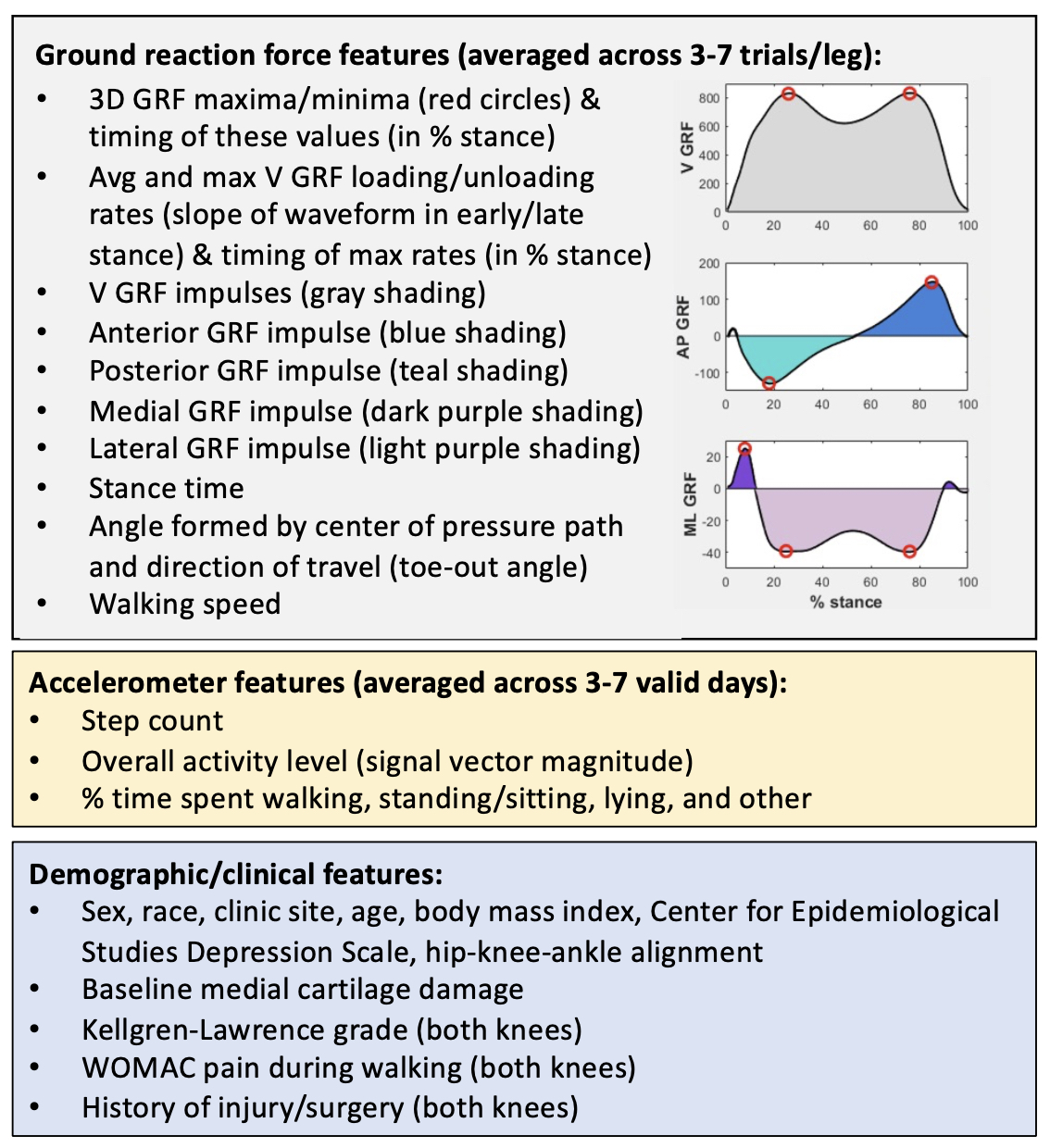
Methods: Demographic and clinical data, ground reaction force (GRF) data during self-selected speed walking, and physical activity data from 7 days of accelerometer wear were collected from participants with and without knee pain or radiographic OA at baseline. Cartilage damage was assessed using the MRI Osteoarthritis Knee Score (MOAKS) in one knee per person by two musculoskeletal radiologists in 5 medial tibiofemoral subregions at the baseline and 2-year visits. Progression was defined as worsening cartilage size or depth MOAKS score in any subregion. Knees with Kellgren-Lawrence grades > 2 were excluded to focus on an earlier disease stage. “Super learning” (an ensemble machine learning approach) was used to predict cartilage worsening over 100 random splits into 70% training:30% test data from standardized GRF, accelerometer, and demographic/clinical features (Figure 1). Performance was evaluated using AUC. Important predictors were identified as the 10 features most frequently appearing in the top 10 contributors to prediction (via a variable importance measure statistic) across the 100 data splits. Marginal effects plots were used to determine direction of associations.
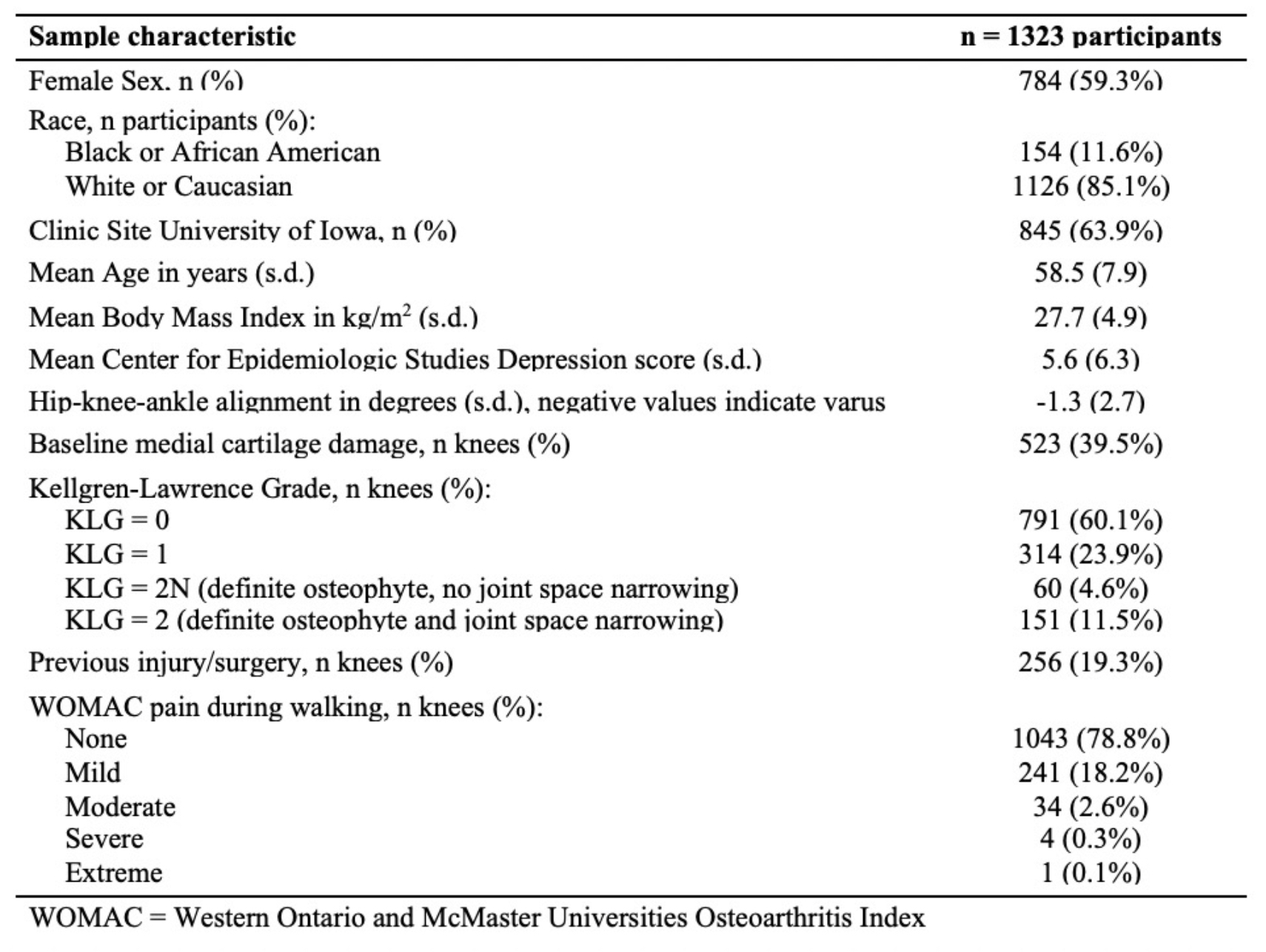
Results: Of 1323 legs included in the analysis (Table 1), 14% experienced medial cartilage worsening over 2-years. Across 100 model runs, the median AUC (2.5- and 97.5-th percentiles) on the held-out test sets was 0.78 (0.73-0.85). Important predictors (frequency of appearance in top 10 contributors) included: baseline medial cartilage damage (100), Kellgren-Lawrence grade (83), % time walking (80), % time sitting/standing (65), age (65), % time lying (62), % time in other activities (61), activity level (54), medial GRF impulse (37), and stance time (31). Cartilage worsening was associated with lower % time walking, % time sitting/standing, and activity level, higher % time lying and medial GRF impulse, and longer stance time (Figure 2).
Conclusion: An ensemble machine learning approach incorporating gait, physical activity, and clinical/demographic features showed good performance for predicting cartilage worsening over two years. While determining the relationships among predictors and cartilage loss outcome in the model is not straightforward, this analysis suggests that addressing low time spent walking and overall activity level and/or high medial GRF impulse, among others, may be potential targets to reduce medial tibiofemoral cartilage worsening.
To cite this abstract in AMA style:
Costello K, Felson D, Jafarzadeh S, Segal N, Lewis C, Nevitt M, Lewis C, Kolachalama V, Kumar D. Using Machine Learning to Predict Medial Knee Cartilage Worsening over 2 Years Using Gait and Physical Activity: The MOST Study [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/using-machine-learning-to-predict-medial-knee-cartilage-worsening-over-2-years-using-gait-and-physical-activity-the-most-study/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/using-machine-learning-to-predict-medial-knee-cartilage-worsening-over-2-years-using-gait-and-physical-activity-the-most-study/