Session Information
Title: Systemic Sclerosis, Fibrosing Syndromes and Raynaud's - Pathogenesis, Animal Models and Genetics
Session Type: Abstract Submissions (ACR)
Background/Purpose
Clinical diversity in systemic sclerosis (SSc) suggests complex multifaceted pathogenesis involving interplay of growth factors or cytokines within the lesional microenvironment. We analysed dermal suction blister fluid to investigate protein expression in skin of SSc patients and healthy controls. We compared the levels of key candidate proteins that may be relevant to pathogenesis.
Methods
Blister fluid (BF) samples from the forearm skin of patients (n=25; DcSSc =19, LcSSc=6) or healthy controls (HC)(n=10) were collected using a dermal suction blister method with paired serum samples, and profiled by Luminex array. Permutation analysis was used for statistical testing.
Results
BF: Profiling showed increased inflammatory cytokines (mean IL-6 in SSc- 77.2 pg/ml, HC-17.8 pg/ml, p=0.009, mean IL-17 in SSc-0.61 pg/ml, HC- 0 pg/ml, p=0.03), and vascular growth factors (PDGF-aa 16.4 pg/ml in SSc, HC-0.97 pg/ml, p=0.049). Additionally MCP-3 (CCL7), IL-15 and IFN-g were all significantly increased in SSc (p<0.05). Plasma: 19/26 SSc patients, and 8/10 HCs were available. Proteins that were significantly raised (p<0.05) in plasma compared to HC, that were also raised in BF were MCP-3 (p=0.025), IL-15 (p=0.02) and IL-6 (p=0.04). Also raised in plasma were IL-1Rα, IL-1a, IL-12p40, GM-CSF, IL-2, IL-4, IL-9, Flt-3L and VEGF (all p<0.05). Of interest Th2 cytokines IL-4, 5, and 13, were only detectable in SSc plasma.
Proinflammatory cytokines (IL-6 (p=0.23), IL-17 (p=0.56)), and growth factors (VEGF(,p=0.47), PDGF(p=0.22)) showed no correlation between serum samples and BF. The healthy controls showed greater correlation between BF and serum, often reaching significance (IL-10,MCP-3,IL1ra,FGF-2).
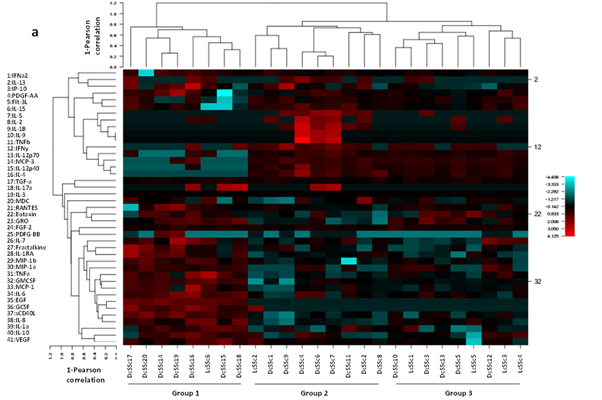
Heatmaps of BF (Figure 1). Unbiased BF analysis by CIMminer (NIH) revealed clustering of SSc patients into 3 groups; Group 1, high IL-6, IL-10, TNFα, and IL-1α high (innate) consisted of mainly early DcSSc with high skin score. Group 2 comprised late stage DcSSc with increased levels of IFNγ, IL-2, IL-4, IL-5, MCP-3, IL12p40, IL12p70 (adaptive). Group3 quiescent with low levels of cytokines and chemokines, and LcSSc or DcSSc patients with low skin score. Plasma analysis did not cluster into distinct clinical groups. ANOVA showed significant difference between skin scores (p=0.003), with Scheffe post hoc analysis showing significant higher skin scores in Group 1 (p=0.005).
Conclusion
Our results confirm the value of dermal blister analysis in SSc, and identify key factors expressed locally. Whilst plasma analysis revealed some overlap with the blister fluid analysis, it did not reflect all of the changes present in the dermal microenvironment. This method profiles the local inflammatory process occurring within the skin and complements clinical and gene expression based classification, as well as suggesting markers of disease activity or treatment effect.
Disclosure:
K. E. N. Clark,
None;
H. Lopez,
None;
X. Shiwen,
None;
B. Ahmed Abdi,
None;
G. Martin,
None;
K. Khan,
None;
D. J. Abraham,
None;
C. P. Denton,
None;
R. J. Stratton,
None.
« Back to 2014 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/use-of-multiplex-cytokine-analysis-of-dermal-blister-fluid-to-assess-local-inflammatory-and-immune-activity-in-systemic-sclerosis/