Session Information
Date: Sunday, November 17, 2024
Title: RA – Treatment Poster II
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Interstitial lung disease (ILD) is a severe extra-articular manifestation of rheumatoid arthritis (RA). Abatacept and rituximab are the recommended drugs. JAK inhibitors (JAKi) have demonstrated efficacy in RA. Nonetheless, evidence on efficacy of JAKi in RA-ILD is scarce. Our objective is to assess a) the effectiveness and b) the safety of Upadacitinib (UPA) and other JAKi in RA-ILD patients.
Methods: National multicenter study of RA-ILD patients on treatment with Upadacitinib (UPA), Filgotinib (FILGO) and Tofacitinib (TOFA). We analyzed from baseline the following outcomes: a) forced vital capacity (FVC), b) diffusing capacity of the lungs for carbon monoxide (DLCO), c) chest high resolution computed tomography (HRCT), d) dyspnea (modified Medical Research Council scale), e) arthritis activity (DAS28-ESR), and f) sparing corticosteroids effect.
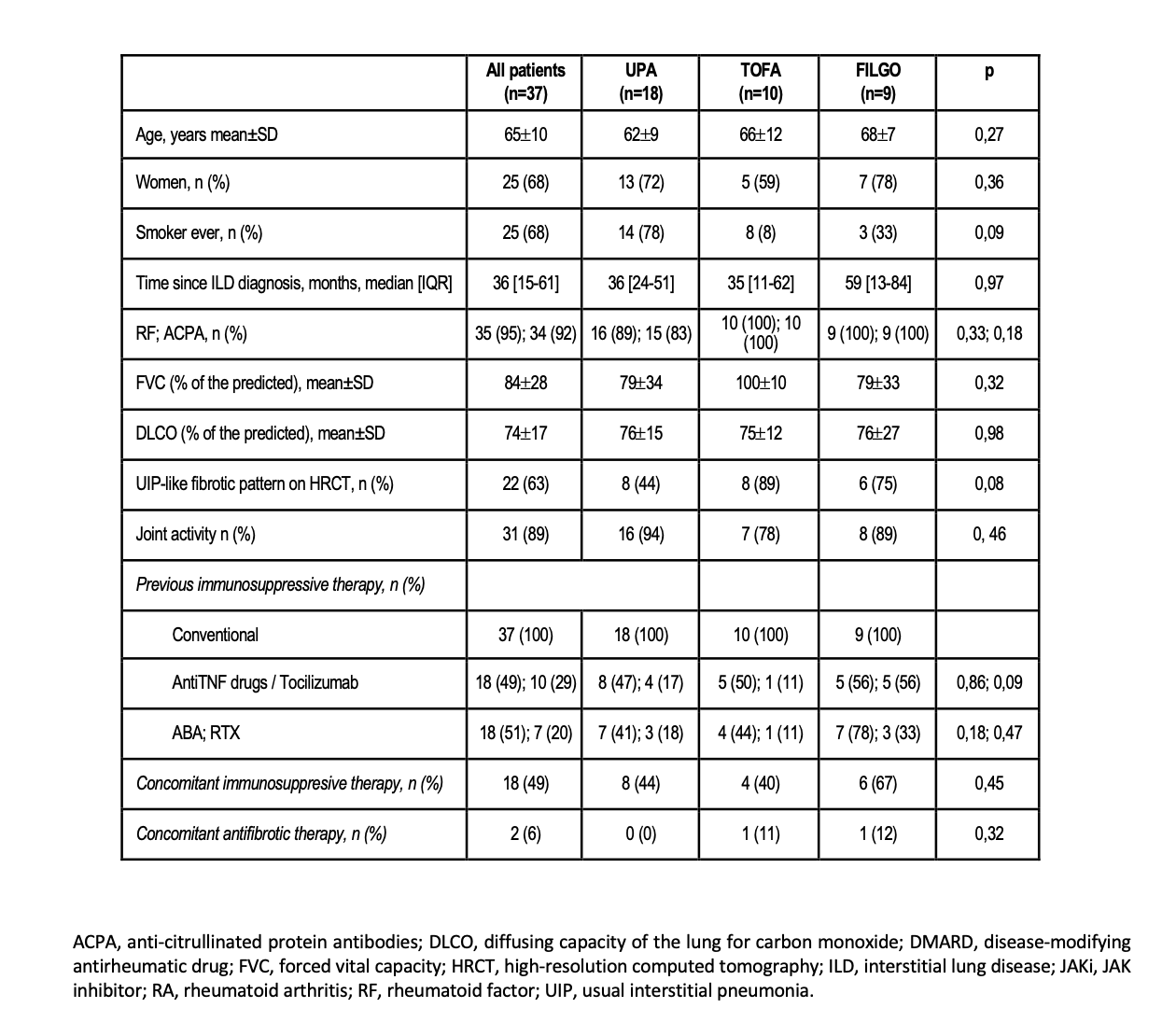
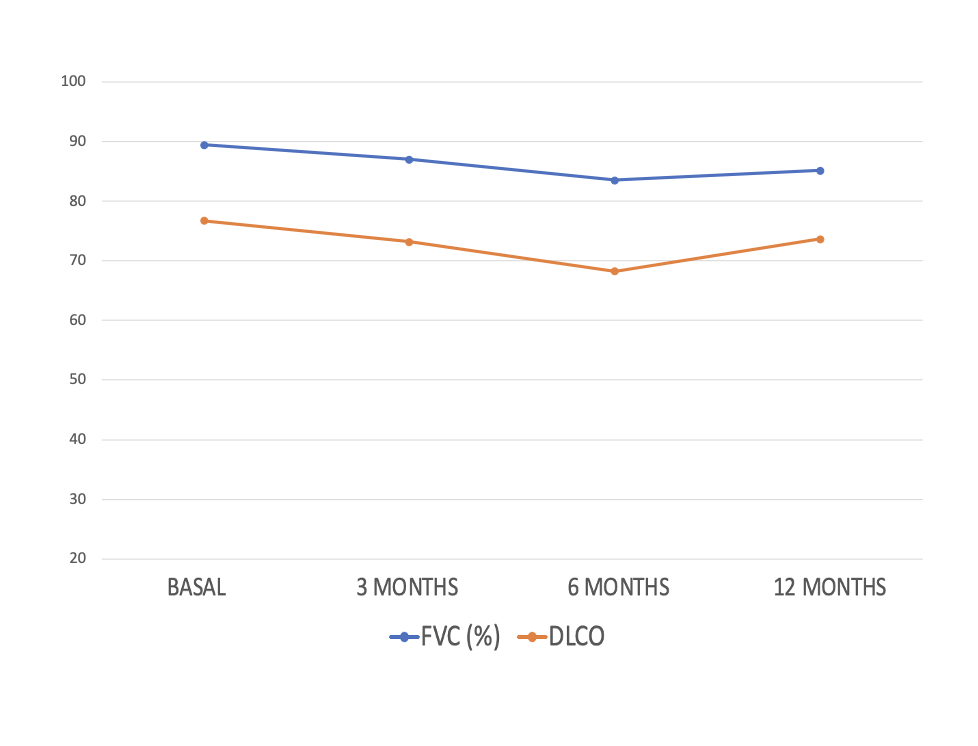
Results: We studied 37 patients (25 women/ 12 men; mean age 65±10 years) from clinical practice on treatment with JAKi [UPA=18 (49%), FILGO= 9 (24%) and TOFA=10 (27%)]. Baseline demographic and clinical characteristics are shown in Table. All patients had received disease-modifying antirheumatic drugs (DMARDs) before JAKi [Conventional (n=37; 100%), anti-TNF (18; 49%), Tocilizumab (10; 29%), Abatacept (18; 51%), and Rituximab (7; 20%)]. Since most patients were on UPA we focused on this group (n=18). Mean baseline values of FVC and DLCO (% predicted) were 79±34 and 76±15, respectively. Patients were followed-up for a median [IQR] of 11 [6-18] months. The evolution of FVC and DLCO remained stable during the first 12 months (Figure). At the end of the follow-up, available chest HRCT images improved/stabilized in all the patients. Stabilization or improvement of dyspnea was found in all the patients. Most patients [10 (67%)] showed articular remission or low activity. UPA was withdrawn in 2 (11%) patients due to zoster virus infection (n=1) and ischemic heart disease (n=1).
Conclusion: JAKi, in this series UPA, may be useful and safe in controlling the course of both pulmonary and joint disease in RA-ILD patients, even in refractory cases to ABA and/or RTX. More studies are needed.
To cite this abstract in AMA style:
Serrano-Combarro A, Atienza-Mateo B, Loarce J, del Olmo Perez L, García-Pérez S, Gonzalez Mozo de Rosales G, Rosas-Gómez de Salazar J, Urruticoechea-Arana A, García-Valle A, Moreno Morales J, Martín López M, Lopez Viejo P, Ruiz-Esquide V, Fernandez Melon J, Castro-Corredor D, Fernández-Ortiz A, Melero-Gonzalez R, Díez Morrondo C, Palma D, del Val del Amo N, Mena Vázquez N, García Dorta A, PÉREZ GALÁN M, MORENO GARCIA M, Blanco-Alonso R. Upadacitinib and Other JAK Inhibitors in the Treatment of Rheumatoid Arthritis – Interstitial Lung Disease. National Multicenter Study Clinical Practice. [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/upadacitinib-and-other-jak-inhibitors-in-the-treatment-of-rheumatoid-arthritis-interstitial-lung-disease-national-multicenter-study-clinical-practice/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/upadacitinib-and-other-jak-inhibitors-in-the-treatment-of-rheumatoid-arthritis-interstitial-lung-disease-national-multicenter-study-clinical-practice/