Session Information
Session Type: Abstract Session
Session Time: 3:00PM-3:15PM
Background/Purpose: Comorbidities are common in patients with rheumatoid arthritis (RA), and comorbidity patterns are of interest. We aimed to examine clusters of comorbidities and clusters of patients based on comorbidities using several methods.
Methods: In this retrospective, population-based study, residents of a geographically well-defined area with prevalent RA on 1-1-2015 were identified from a comprehensive medical record linkage system. Diagnostic codes were retrieved for a 5 year period prior to the prevalence date. Using 2 codes at least 30 days apart, the 44 comorbidities described by England et al (ARD 2020) were defined. Unsupervised machine learning methods of interest included ascendant hierarchical clustering, network analysis, partitioning around medoids and latent class analysis. Methodologic considerations include the research question of interest, whether the method is appropriate for categorical data, method assumptions (e.g., some methods assume equal sample size per cluster), the optimal number of clusters, internal validation, stability and biological plausibility.
Results: A total of 1409 patients with prevalent RA (72% female; 92% white; mean age 63.5 years) were studied. Comorbidities were present in 1187 (84%) of the subjects with 5+ comorbidities present in 749 (53%) subjects.
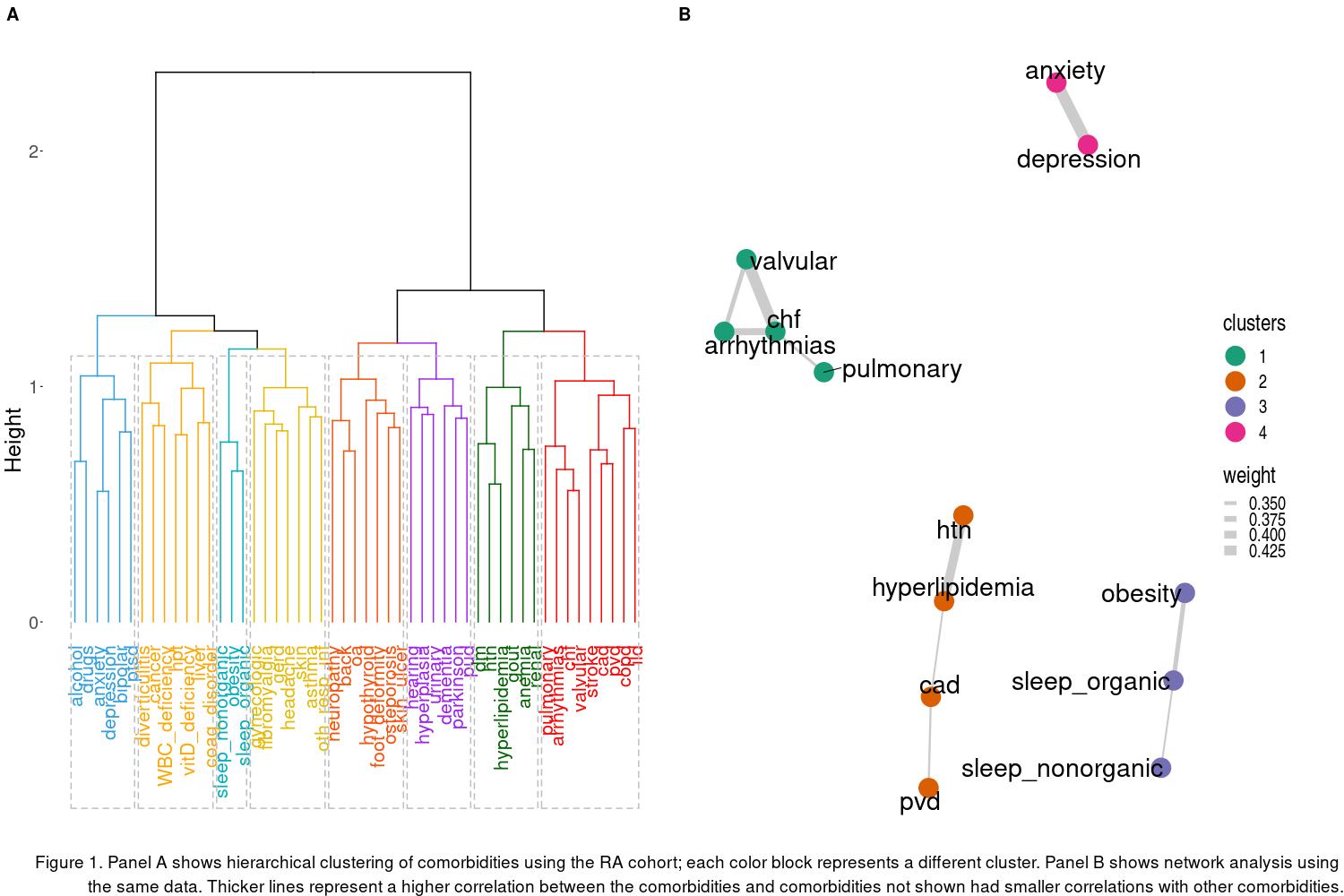
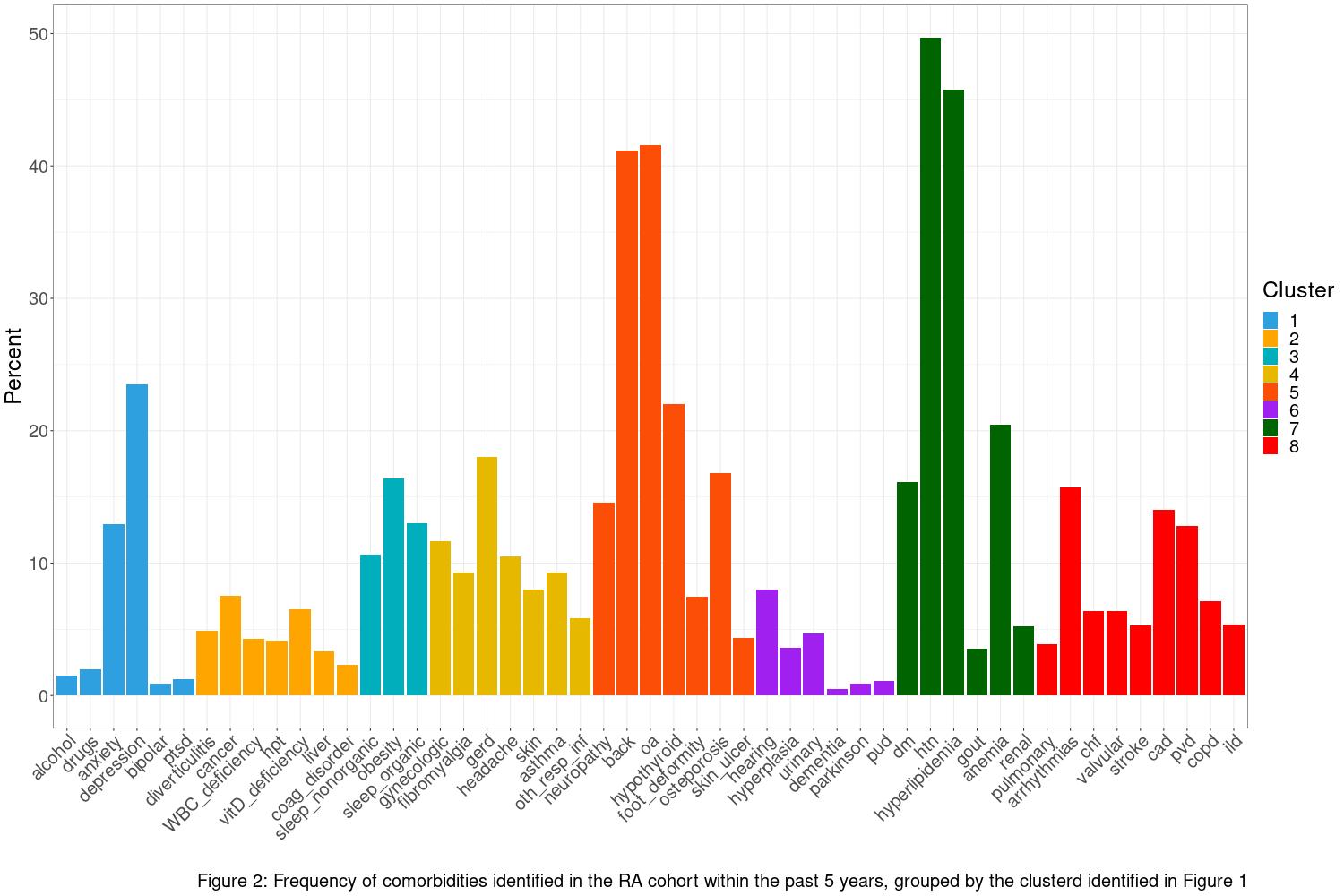
Clustering of comorbidities using hierarchical clustering methods yielded 8 clusters (Figure 1a) while network analysis (Figure 1b) yielded 4 clusters. In both methods, the clusters were primarily organized around body systems (e.g., cardiovascular, respiratory, mental/behavioral comorbidities) with greater stability between methods for comorbidities with higher prevalence than those that were less common. Figure 2 illustrates the prevalence of each comorbidity within the cohort, grouped according to the clusters identified using the hierarchical approach.
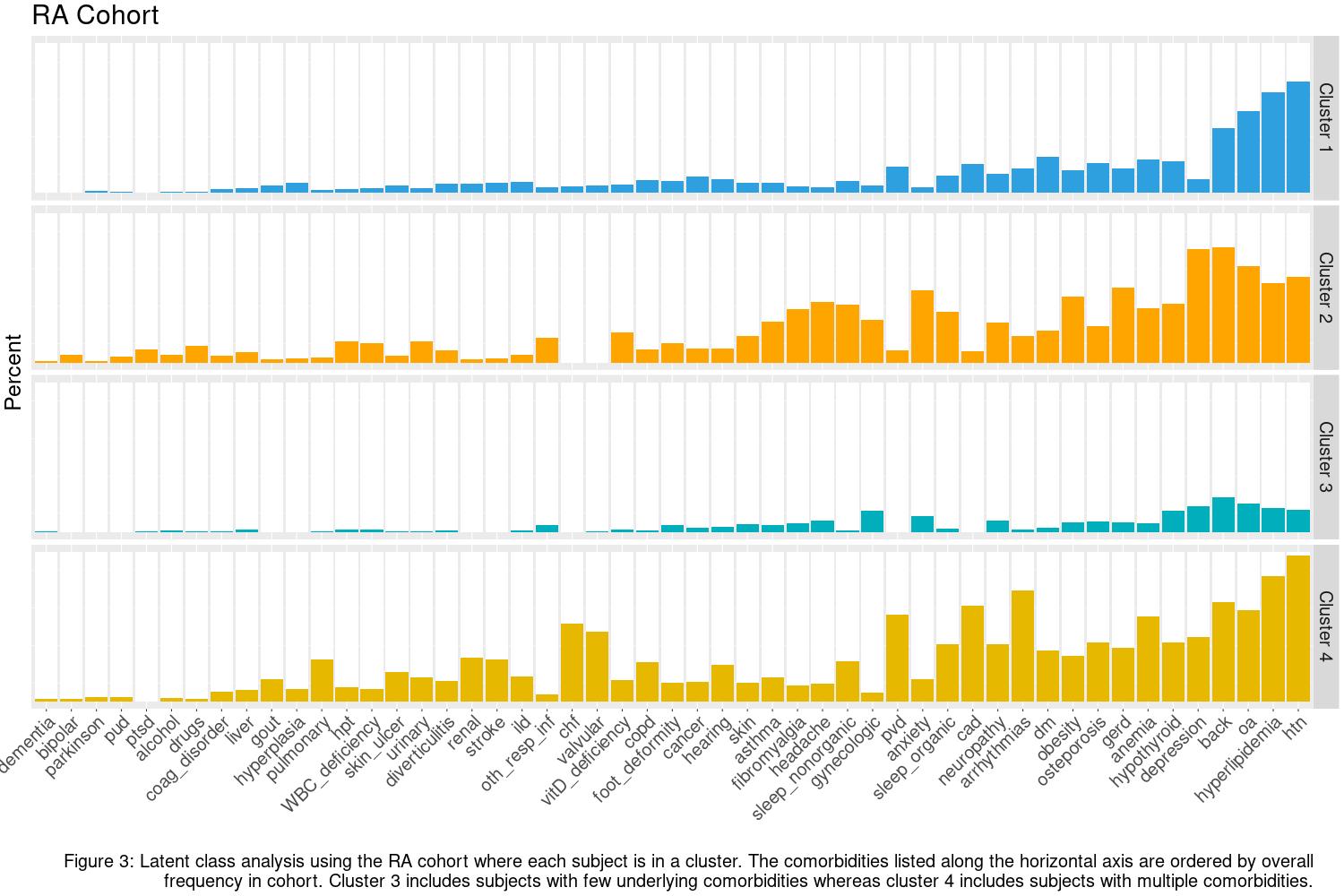
Clustering of patients into subgroups based on comorbidity profiles using partitioning around medoids and latent class analysis yielded groups with no/few comorbidities, many comorbidities, and 2-3 intermediate groups with some comorbidities. Figure 3 shows the prevalence of each comorbidity within the 4 clusters identified using latent class analysis.
Conclusion: Clustering of comorbidities and clustering of patients can provide useful information about multimorbidity patterns in patients with RA. Clustering variables allows for easy application to other cohorts (e.g., non-RA). Clustering of RA subjects primarily created groups of subjects who had varying numbers of comorbidities. Various clustering methods are available, and these methods yield different results. It is important to understand the assumptions of these methods, as well as how to determine the optimal number of clusters for each method. Further research is needed to determine the best methods for identifying comorbidity patterns in RA.
To cite this abstract in AMA style:
Atkinson E, Gunderson T, Davis J, Myasoedova E, Kronzer V, Coffey C, Crowson C. Unsupervised Machine Learning Methods to Cluster Comorbidities in a Population-based Cohort of Patients with Rheumatoid Arthritis [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/unsupervised-machine-learning-methods-to-cluster-comorbidities-in-a-population-based-cohort-of-patients-with-rheumatoid-arthritis/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/unsupervised-machine-learning-methods-to-cluster-comorbidities-in-a-population-based-cohort-of-patients-with-rheumatoid-arthritis/