Session Information
Date: Monday, November 8, 2021
Session Type: Poster Session C
Session Time: 8:30AM-10:30AM
Background/Purpose: Previous research in axial spondyloarthropathy(axSpA) has shown this population to have a high prevalence of depression. This co-morbidity has been previously shown to impact disease activity in patients with rheumatic disease.
The purpose of this study was to screen for early signs of depression using two validated tools, the Patient Health Questionaire-9 (PHQ-9) and the Hospital Anxiety and Depression Scale for depression (HADs-D) in patients with known axSpA.
Methods: AxSpA patients attending the Rheumatology department in St James’ Hospital between February and October 2020 were invited to take a self-administered survey which included the PHQ-9 and the HADs-D. Scores from the HADs-D yielded a numerical result which was then categorised as normal, borderline or abnormal. PHQ-9 numerical results were categorised as normal, mild, moderate, moderate/severe or severe. Patients with a known diagnosis of depression were excluded. In addition to baseline demographics, patient reported outcomes from the clinic visit were also recorded.
Data analysis was performed using IBM SPSS version 26. Continuous variables were recorded as means, categorical variables as frequencies with percentages. A one-way analysis of variance analysis (ANOVA) was used to determine significance of variation in outcomes between patient outcomes as determined by the HADs-D and PHQ-9. A p-value of < 0.05 was deemed significant. Informed consent was obtained prior to participation. Approval for this study was received from the St James’/Tallaght Hospital Joint Ethics Committee.
Results: In total 71 axSpA patients took part in the survey. The population was 70.4%(50) males and 29.5%(21) female, with an average age 47.9 years and mean disease duration 19.7 years (mean outcomes: BASDAI 4.08, BASFI 3.62, BASMI 3.54, ASQoL 6.79). Overall, 7 (9.9%) participants recorded abnormal HADs-D scores, while 17 (23.9%) recorded moderate to severe PHQ-9 scores indicative of underlying depression. AxSpA females had higher mean HADs-D scores (7.5 vs 4.8, p=0.01) than males, with abnormal scores in 19%(4) of females and 6% (3) of males. No significant differences were found in PHQ-9 scores between genders.
Analysis revealed significantly worse BASDAI (6.27 vs 3.42, p< 0.01) and AQoL scores (12.57 vs 5.26, p< 0.01) in axSpA patients with abnormal compared to normal HADs-D scores (figure 1). No significant differences were noted in BASFI, BASMI or baseline demographics. A similar pattern was noted on analysis of PHQ-9 scores, with significantly worse BASDAI (7.9 vs 2.55, p< 0.01), BASFI (8.05 vs 2.33, p< 0.01) and ASQoL (19.5 vs 2.62, p< 0.01) noted in those scoring as severe compared to normal (figure 2). No significant differences were detected in BASMI scores or baseline demographics.
Conclusion: A high percentage of axSpA patients recorded high HADs-D and PHQ-9 scores concerning for undiagnosed depression. These patients were noted to have significantly worse disease activity and quality of life as compared to patients with normal scores. Clinicians treating axSpA should consider actively screening for depression in this population.
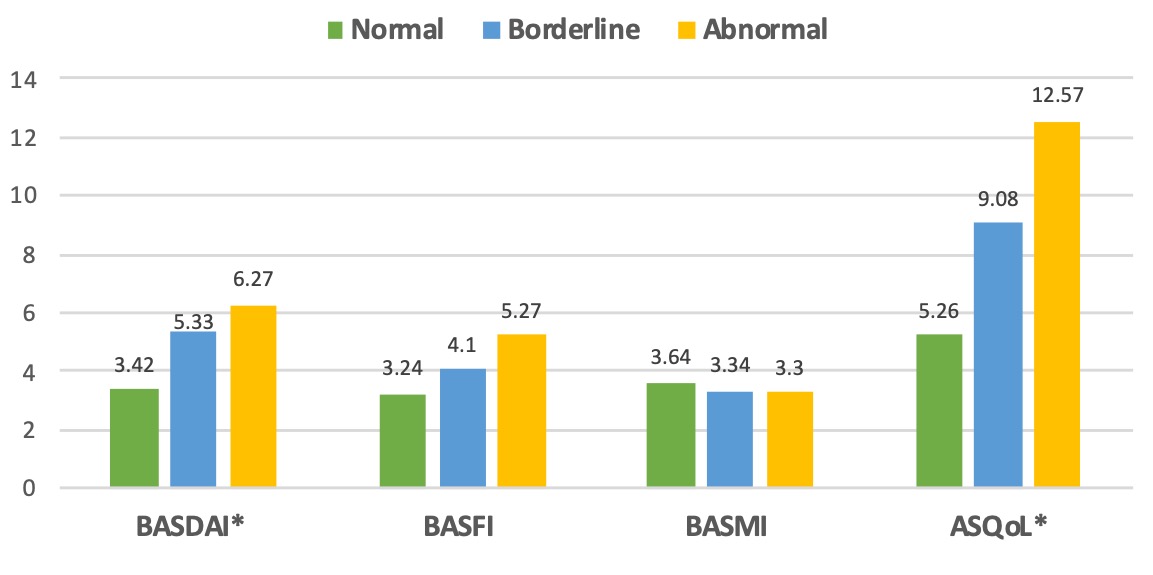 Figure 1: Patient outcomes by HADs-D scores (*indicates significant differences at the p < 0.05 level)
Figure 1: Patient outcomes by HADs-D scores (*indicates significant differences at the p < 0.05 level)
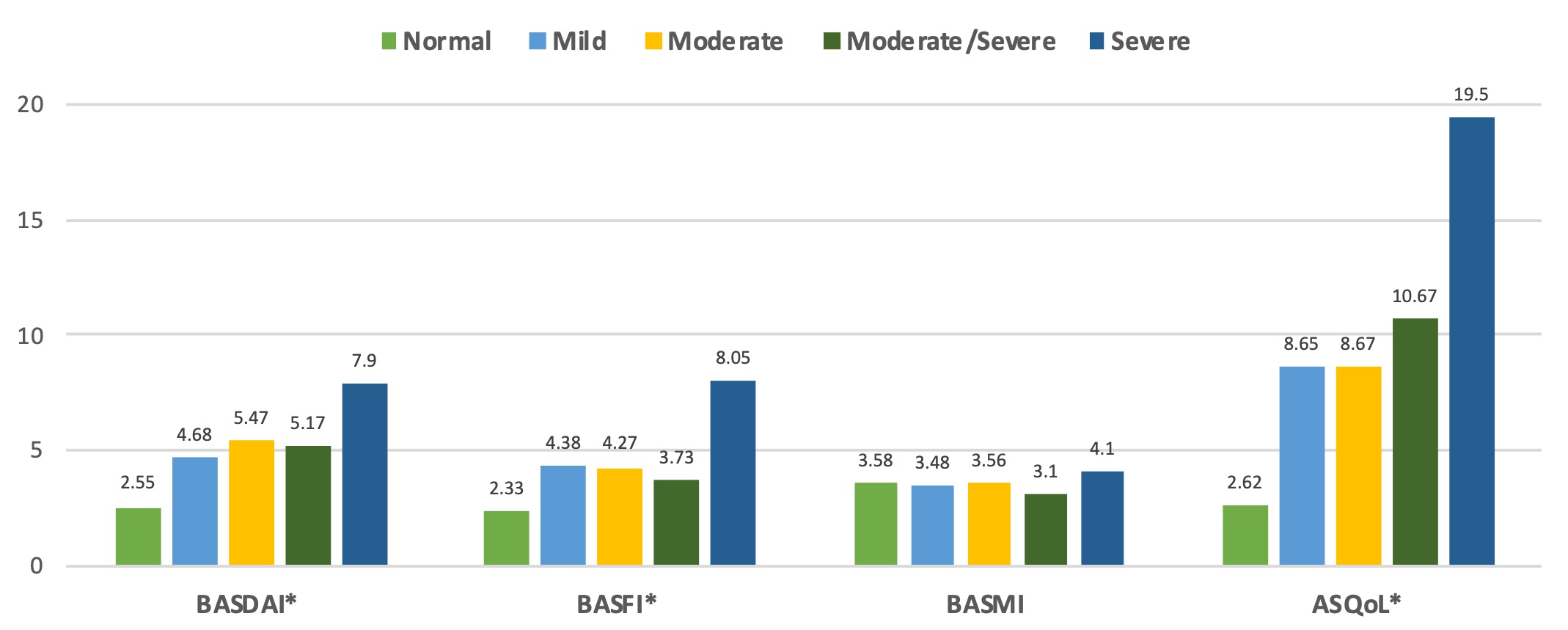 Figure 2: Patient outcomes by PHQ-9 scores (*indicates significant differences between normal, mild and severe groups at the p < 0.05 level)
Figure 2: Patient outcomes by PHQ-9 scores (*indicates significant differences between normal, mild and severe groups at the p < 0.05 level)
To cite this abstract in AMA style:
Maguire S, Gallagher P, O'Shea F. Undiagnosed Depression in Axial Spondyloarthropathy and the Negative Impact on Patient Outcomes: Results of a Screening Study [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/undiagnosed-depression-in-axial-spondyloarthropathy-and-the-negative-impact-on-patient-outcomes-results-of-a-screening-study/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/undiagnosed-depression-in-axial-spondyloarthropathy-and-the-negative-impact-on-patient-outcomes-results-of-a-screening-study/
