Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: The complement (C) system has been associated with the etiopathogenesis of rheumatoid arthritis (RA). Insulin resistance (IR) and metabolic syndrome are prevalent among RA patients. The aim of this study was to explore the relationship between a comprehensive evaluation of the C system and IR, as well as metabolic syndrome, in RA patients.
Methods: 339 non-diabetic patients with RA were recruited. Functional assays of the three C pathways were assessed. Additionally, serum levels of individual components of the C system were measured: C1q (classical), lectin (lectin), C2, C4, and C4b (classical-lectin), factor D and properdin (alternative), C3 and C3a (common), C5, C5a, and C9 (terminal), as well as regulators factor I and C1-inhibitor. IR and beta cell function indices were calculated using the homeostatic model assessment (HOMA). Criteria for metabolic syndrome were applied. Multivariable linear regression analysis was performed to investigate the association between the C system and IR in RA patients.
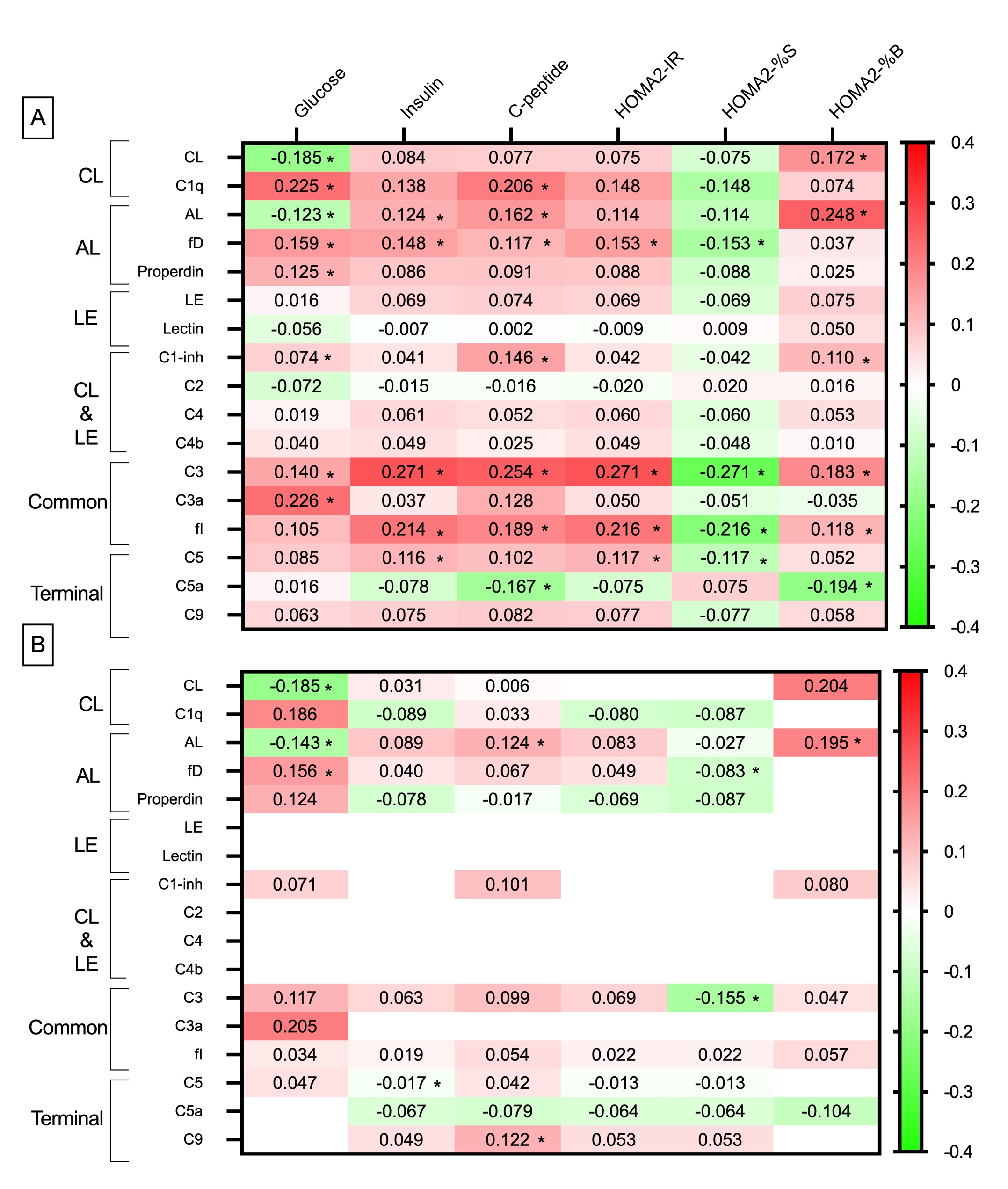
Results: Spearman’s rho correlation heatmap analysis of C system pathways and IR indices is shown in Figure 1-A. In this univariable analysis, multiple significant associations were found. Most of these associations were positive (depicted in red on the correlation map). Regarding C functional tests, the classical pathway exhibited a significant negative relationship with plasma glucose levels and a positive correlation to the HOMA2-%B index. The alternative pathway showed the same associations as the classical pathway but also disclosed significant positive associations with serum insulin and C-peptide levels. Remarkably, the functional test of the lectin pathway did not show statistically significant associations with any glucose homeostasis parameter.
In terms of the C system molecules, most associations were identified for molecules situated at the upper and common segments of both the classical and alternative pathways, rather than for those within the lectin pathway or the terminal cascade of the C system (Figure 1-A). In the correlation heatmap presented in Figure 2-A, only associations with a p-value lower than 0.20 from Figure 1-A were subsequently adjusted for confounders and expressed as standardized beta coefficients. After this adjustment for covariates, most of the associations from the univariable analysis lost significance (Figure 1-B). Only the positive relation between the alternative route functional test and C-peptide and HOMA2-%B retained its significance.
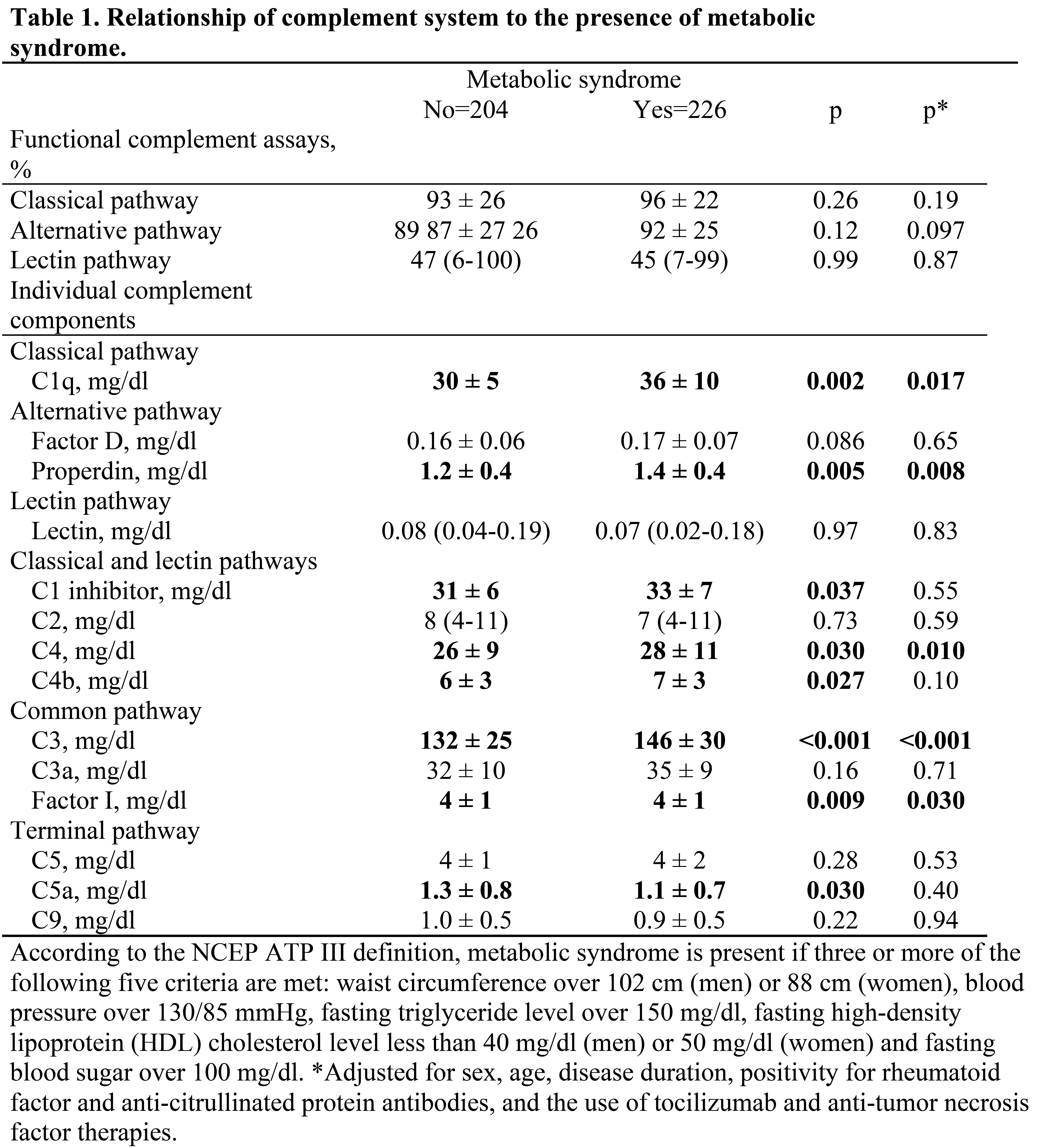
Differences in C values between patients with and without metabolic syndrome is shown in Table 1. Although the functional C tests corresponding to the three cascades did not significantly differ between the groups, the values of C1q, properdin, C4, C3, and factor I were significantly higher in patients with metabolic syndrome compared to those without it after multivariable adjustment.
Conclusion: There is a positive correlation between the complement system and metabolic syndrome among non-diabetic patients with RA. This association is independent of traditional IR factors.
To cite this abstract in AMA style:
Viotti-Serra J, Garcia-Gonzalez M, Gomez-Bernal F, Quevedo-Abeledo J, Gonzalez-Gay M, Ferraz-Amaro i. Understanding the Role of the Complement System in Insulin Resistance and Metabolic Syndrome in Patients with Rheumatoid Arthritis [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/understanding-the-role-of-the-complement-system-in-insulin-resistance-and-metabolic-syndrome-in-patients-with-rheumatoid-arthritis/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/understanding-the-role-of-the-complement-system-in-insulin-resistance-and-metabolic-syndrome-in-patients-with-rheumatoid-arthritis/