Session Information
Session Type: Poster Session (Tuesday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Photosensitivity resulting in inflammatory skin lesions is a hallmark of cutaneous lupus. Lesions can be disfiguring and have a negative impact on patients’ quality of life. Understanding photosensitivity is critical to developing better treatment. Prior research by our lab showed that ADAM17, a metalloprotease found on Langerhans cells (LCs), is activated by ultraviolet radiation (UVR) and is critical for limiting UVR-induced keratinocyte apoptosis and skin inflammation through cleavage and activation of epidermal growth factor receptor (EGFR) ligands. Two photosensitive lupus models showed reduced LC ADAM17 expression with evidence for dysfunction in human lupus, suggesting that photosensitivity is at least in part due to dysfunctional LCs. We propose a cross-sectional study to evaluate the hypothesis that LC ADAM17 expression and activity are reduced in the epidermis of lupus patients, contributing to photosensitivity. Our secondary hypothesis addresses whether reduced ADAM17 expression and increased photosensitivity is associated with lupus disease activity and severity. As part of our secondary hypothesis, we will correlate reduced ADAM17 levels with increased type I interferon (IFN) in lupus.
Methods: Transcriptomics of non-lesional skin from discoid lupus (DLE) and healthy controls were compared using microarray. Data was gathered from unpublished data from Krueger et al (2014) looking at immune related pathways present in DLE lesions compared to psoriasis and healthy skin. This study showed an enrichment of IFN gamma associated genes in DLE. We plan to collect punch biopsies of non-lesional, non-sun exposed skin from 10 patients who meet ACR/SLICC criteria for lupus nephritis as well as 5 healthy controls, at a single visit. We will perform flow cytometry on LCs from these biopsies to assess ADAM17 expression and activity. We will collect the SLE Disease Activity Index (SLEDAI) and will evaluate the correlation between ADAM17 activity with disease activity. Lastly, we will perform RNA sequencing to evaluate the IFN signature and correlate IFN expression with ADAM17 levels.
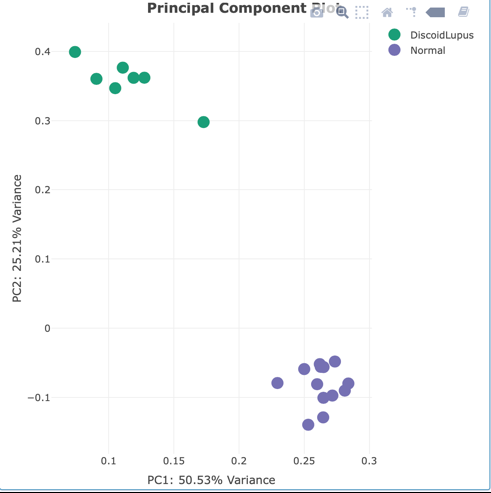
Results: Principal component analysis of microarray results demonstrated the variance between non lesional DLE skin and controls (Fig 1). Expression of IFN related genes were found to be elevated in non-lesional skin versus controls (Fig 2). Genes found to be highly expressed in non-lesional DLE skin included S100A12 and OASL(Fig 3). These results suggest an elevated IFN signature and inflammatory markers in non-lesional skin of DLE patients. We also demonstrate we can successfully assay for LC ADAM17 levels by 13 parameter flow cytometric analysis of human skin biopsies, and preliminary results from analysis of SLE patients are expected in the next several months.
Conclusion: Microarray results suggest an elevated IFN signature in non-lesional skin of DLE patients. If we find ADAM17 expression is reduced in non-lesional skin of SLE nephritis patients in comparison to controls, this would support a role of ADAM17 and perhaps type I IFN in SLE photosensitivity. These findings could lead to targeting of ADAM17 and potentially of type I IFN for treating the photosensitive rash seen in patients with lupus.
To cite this abstract in AMA style:
Lu T, Schwartz N, Li T, Shipman W, Dasoveanu D, Liu Y, Anandasabapathy N, Lee H, Jabbari A, Krueger J, Mehrara B, Veiga K, Minkis K, Oliver D. Understanding Langerhans Cell ADAM17 Levels in Systemic Lupus Erythematosus: Potential Contributor to Photosensitivity [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/understanding-langerhans-cell-adam17-levels-in-systemic-lupus-erythematosus-potential-contributor-to-photosensitivity/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/understanding-langerhans-cell-adam17-levels-in-systemic-lupus-erythematosus-potential-contributor-to-photosensitivity/