Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Current classification criteria of lupus nephritis (LN) emphasize glomerular pathology, however tubular atrophy and interstitial fibrosis (TAIF) are better predictors of poor renal outcomes.1 In this work, we evaluate tubulointerstitial inflammation (TII) as a risk factor for TAIF and renal failure.
Methods: The subset of LN patients that underwent ≥2 renal biopsies, because of persistent or recurrent LN, at Columbia University Medical Center (CUMC) from 1994-2018 were identified. All renal biopsies were interpreted by nephropathologists at the CUMC Department of Pathology and classified using the ISN/RPS LN classification criteria. OPAL multiplex immunohistochemistry staining to identify CD3, CD4, CD8, CD19 and CD68 expression in the kidney tissue was performed.
Results: 104 LN patients (84% female, 25±12 years old at diagnosis, 14% White, 40% Black, 35% Hispanic) requiring sequential renal biopsies with a median follow-up of 11 [6-16] years were identified. On initial biopsy, 94/104 (90%) had class III or IV proliferative LN with or without class V. Forty-seven (51%) patients developed ESRD. Nine patients died and 14 were lost to follow-up.
Multivariable modeling of histopathological findings on biopsy 1 identified the presence of crescents to be associated with progression to ESRD (OR 3.14 95% CI 1.22, 8.08), while the presence of wire-loop lesions was protective (OR 0.28 98% CI 0.09, 0.85). On biopsy 2, the presence of TAIF≥25% (OR 4.50, 95% CI 1.30, 15.55) and glomerulosclerosis in >25% of glomeruli (OR 3.78, 95% CI 1.15, 0.03) were the only independent predictors of ESRD.
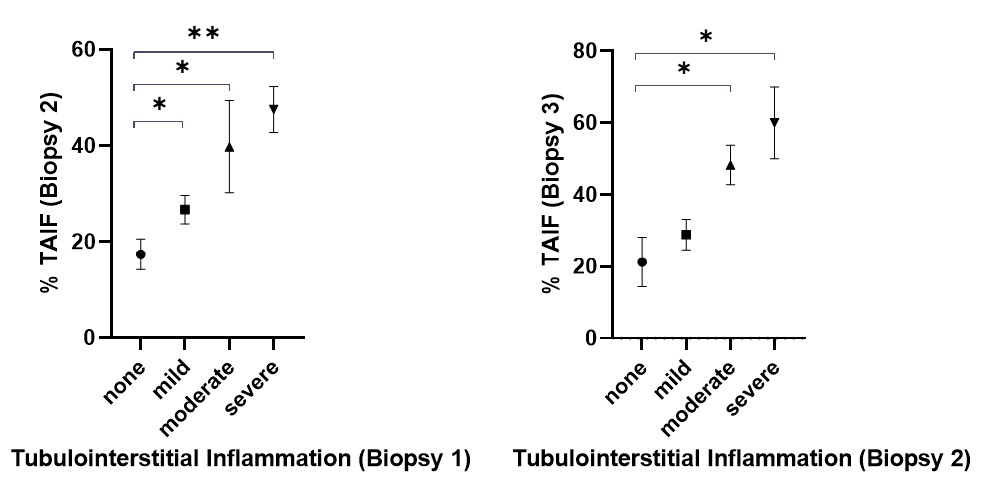
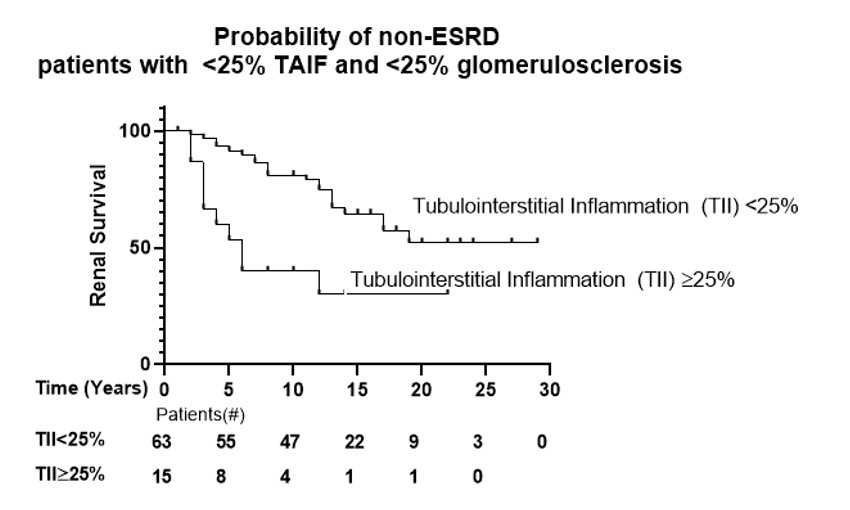
There was a sequential increase in TAIF severity on successive biopsy samples (10%, 26%, 34%, and 46% TAIF on biopsy 1 through 4, respectively). On univariable analysis, TAIF≥25% biopsy 2-4 predicted progression to ESRD (p< 0.01). The severity of TII on biopsy 1 was associated with increased risk of more advanced TAIF on biopsy 2, while TII on biopsy 2 predicted TAIF on biopsy 3, (Fig 1). Interestingly, in the 78 patients with < 25% TAIF and < 25% sclerotic glomerular involvement, moderate-severe TII significantly predicted ESRD (OR 4.76 95% CI 1.68, 13.50), (Fig 2).
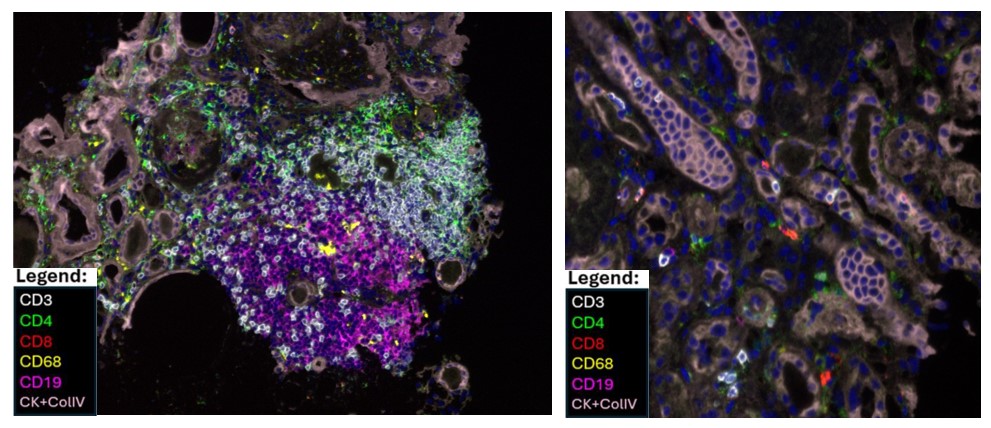
Multiplex immunohistochemistry staining of kidney biopsy samples revealed that TII could be detected as organized immune infiltrate of T cell rich and B cell rich areas reminiscent of tertiary lymphoid structures (Fig 3, left) or as tubulitis mediated by CD3 T cells, often CD4neg and CD8neg (Fig 3, right).
Conclusion: TII predicts the development and extent of TAIF in lupus nephritis and is associated with a higher risk of progression to ESRD.
ACKNOWLEDGEMENT: The authors gratefully acknowledge the support of Dr. Anca D. Askanase and Dr. Adam Mor in this work.
1. Hsieh C et al. Predicting outcomes of lupus nephritis with tubulointerstitial inflammation and scarring. Arthritis Care Res (Hoboken). 2011 Jun;63(6):865-74.
To cite this abstract in AMA style:
Gartshteyn Y, Geraldino L, Wang S, D'Agati V, Winchester R. Tubulointerstitial Inflammation Predicts Tubular Atrophy, Fibrosis, and Renal Function Loss in Lupus Nephritis [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/tubulointerstitial-inflammation-predicts-tubular-atrophy-fibrosis-and-renal-function-loss-in-lupus-nephritis/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/tubulointerstitial-inflammation-predicts-tubular-atrophy-fibrosis-and-renal-function-loss-in-lupus-nephritis/