Session Information
Date: Sunday, November 7, 2021
Title: RA – Diagnosis, Manifestations, & Outcomes Poster II: Miscellaneous Aspects of RA (0786–0812)
Session Type: Poster Session B
Session Time: 8:30AM-10:30AM
Background/Purpose: Self-efficacy (SE), or patients’ confidence in their ability to control disease and its consequences, was recently prioritised in EULAR-recommendations for self-management strategies for inflammatory arthritis (1). However, it remains unclear which factors influence SE in rheumatoid arthritis (RA), particularly during early disease.
Methods: We conducted a post-hoc analysis of the 2-year RCT Care in early RA (CareRA), which studied remission-induction treatment regimens for early RA. Participants completed the Arthritis Self-Efficacy Scale (ASES), Short Form 36 (SF-36), Revised Illness Perception Questionnaire (IPQ-R), Utrecht Coping List (UCL), RAQoL and Health Assessment Questionnaire (HAQ). Depending on time to first remission (DAS28-CRP < 2.6) and persistence of remission, treatment response was defined as persistent response, secondary failure, delayed response, late response or non-response. The association between ASES scores and clinical/psychosocial factors was explored with Spearman correlation and multivariate linear mixed models. Baseline predictors of week 104 ASES were identified with exploratory simple linear regression followed by multiple linear regression of significant predictors adjusted for DAS28-CRP, HAQ, treatment arm, treatment response and demographic/serologic confounders. Models were adjusted for multiple comparisons, setting significance at a = 0.003.
Results: All 379 patients had a recent diagnosis of RA and were DMARD-naïve at study initiation. Most patients were women (69%) and RF/ACPA-positive (66%) and the mean (SD) age was 52 (13) years. For all tested outcome measures, better perceived health correlated with higher SE (Table 1). While patient-reported factors (HAQ, SF-36, RAQoL, IPQ-R, pain, fatigue and patient global assessment) showed moderate/strong correlations with ASES scores, correlations with physician-reported factors (physician global assessment, SJC28), TJC28 and DAS28-CRP were weak. In mixed models, only more favourable outcomes on patient-reported factors and DAS28-CRP were associated with higher ASES scores at each time point.
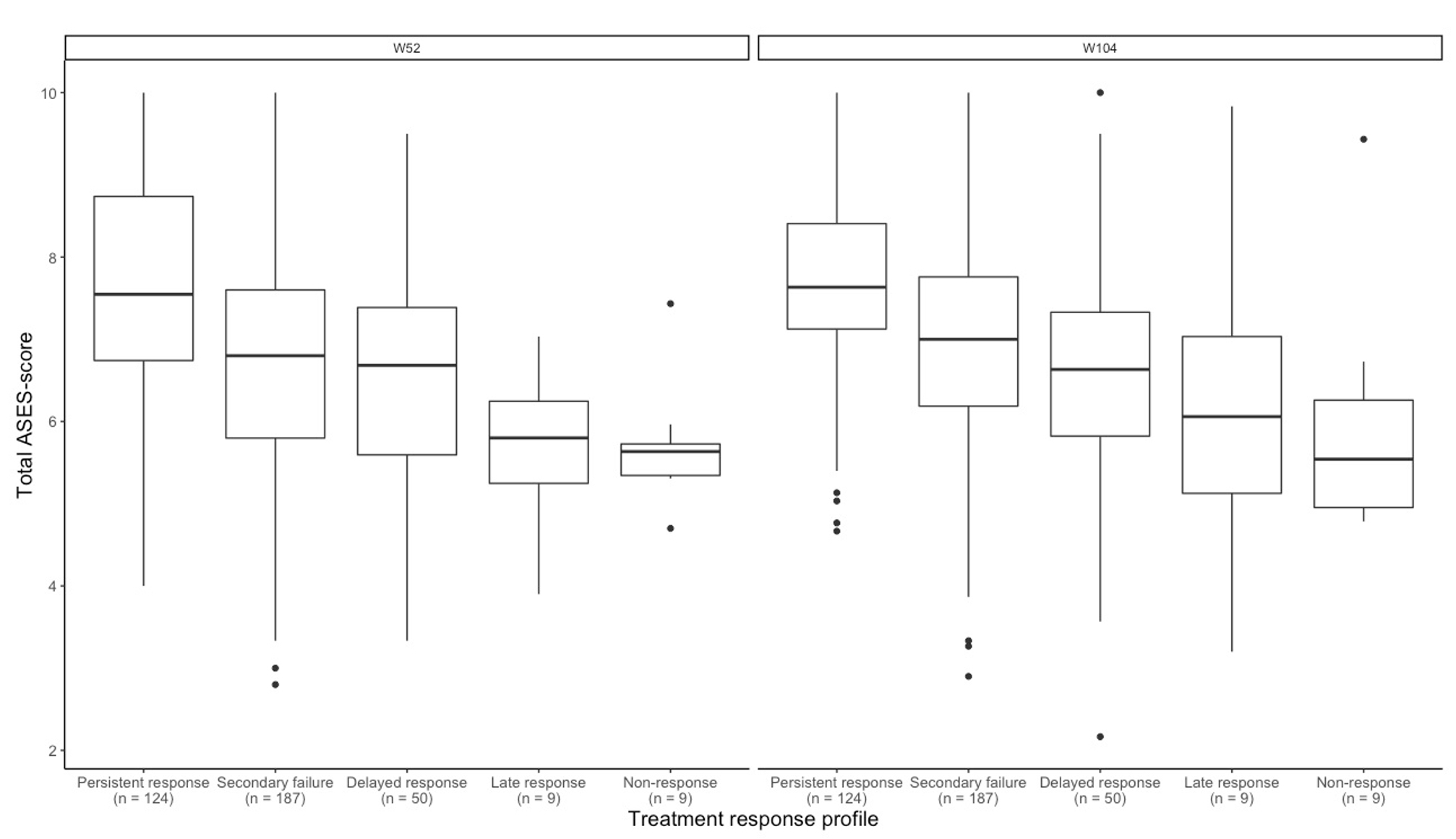
An earlier, persistent treatment response predicted higher ASES scores at both week 52 and 104 (Fig. 1). Significant baseline predictors of week 104 ASES included HAQ; SF-36 dimensions Mental Component Score, Vitality, Mental Health and Role Emotional; IPQ-R dimensions Illness coherence, Treatment control, Emotional representations and Consequences; UCL dimension Passive reacting and the RAQoL (Table 2).
Conclusion: Patient-reported outcomes and treatment response were important early determinants of long-term SE in an early RA clinical trial. These results provide further relevance for the window of opportunity in an early treat-to-target strategy. In addition, our results could help to timely identify patients who might benefit the most from self-management treatment strategies or interventions to improve SE. Further prospective research is needed to confirm these findings.
(1) Nikiphorou E, et al. EULAR recommendations for the implementation of self-management strategies in patients with inflammatory arthritis. Ann Rheum Dis 2021
ASES = Arthritis Self-Efficacy Scale; Persistent response = sustained remission from week 16 to week 104; Secondary failure = loss of remission after week 16; Delayed response = first remission after week 16; Late response = first remission after week 52; Non-response = no remission within 104 weeks
Bonferroni-correction for multiple comparisons was applied, setting the significance level at p < 0.003.
ASES = Arthritis Self-Efficacy Scale, DAS28 = Disease Activity Score in 28 joints, HAQ = Health Assessment Questionnaire, VAS = Visual Analogue Scale, PGA = patient global assessment, SF_36 MCS = Short-Form 36 mental component score, IPQ-R = Revised Illness Perception Questionnaire, PhGA = physician global assessment, TJC28 = tender joint count in 28 joints, SJC28 = swollen joint count in 28 joints, CRP = C-reactive protein, ESR = erythrocyte sedimentation rate
Results were obtained from multivariate linear regression models predicting total ASES-score at week 104 by predictors that were significant in univariate analyses, and adjusting for age, gender, treatment arm and response, auto-antibody status and baseline HAQ and DAS28-CRP or its components.
Bonferroni-correction for multiple comparisons was applied, setting the significance level at p < 0.003.
ASES = Arthritis Self-Efficacy Scale, HAQ = Health Assessment Questionnaire, VAS = Visual Analogue Scale, PGA = patient global assessment, PhGA = physician global assessment, SF_36 = Short-Form 36, MCS = mental component score, IPQ-R = Revised Illness Perception Questionnaire, UCL = Utrecht Coping List
To cite this abstract in AMA style:
Doumen M, De Cock D, Pazmino S, Bertrand D, Westhovens R, Verschueren P. Treatment Response and Several Patient-reported Outcomes Are Early Determinants of Future Self-efficacy in Patients with Rheumatoid Arthritis [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/treatment-response-and-several-patient-reported-outcomes-are-early-determinants-of-future-self-efficacy-in-patients-with-rheumatoid-arthritis/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/treatment-response-and-several-patient-reported-outcomes-are-early-determinants-of-future-self-efficacy-in-patients-with-rheumatoid-arthritis/