Session Information
Date: Saturday, April 1, 2023
Session Type: Plenary Session
Session Time: 11:00AM-12:00PM
Background/Purpose: Calcinosis is a poorly understood and morbid complication of juvenile dermatomyositis (JDM). As there is no consensus treatment approach for calcinosis, and limited knowledge of outcomes, we seek to inform future treatment guidance for this significant complication of JDM by performing this multi-institutional retrospective review of treated cases of JDM calcinosis to assess outcomes as they relate to JDM severity, initial treatment, and calcinosis-directed treatment.
Methods: Collaborators of the Childhood Arthritis and Rheumatology Research Alliance (CARRA) submitted retrospectively reviewed cases with data collected at timepoints of JDM and calcinosis diagnoses, respectively, as well as the determined outcome of each specific calcinosis treatment(s). All cases were sourced from electronic health record searches of clinical terms or billing codes. Only cases diagnosed and treated from 2003 to 2019 were included to capture the contemporary era of JDM treatment. Cases were required to have probable/definitive JDM by Bohan and Peter criteria and calcinosis. Outcome was assessed in univariable and multivariable analyses as time to any improvement by clinician judgement utilizing all available follow-up. Proportion with any improvement along with 95% confidence intervals was estimated using Kaplan-Meier analysis. Multivariable Cox models were used to assess the association between patient characteristics and time to any improvement beginning at calcinosis diagnosis.
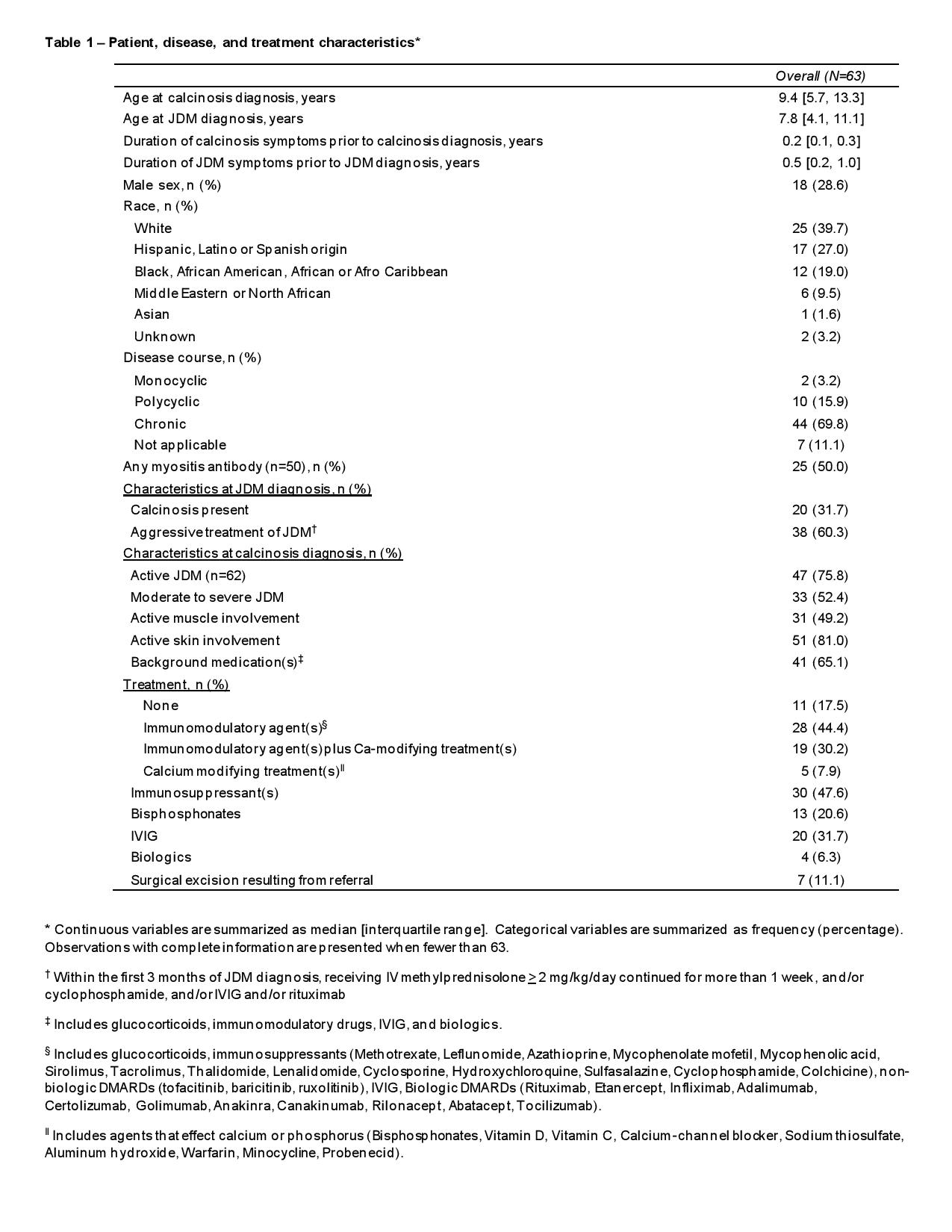
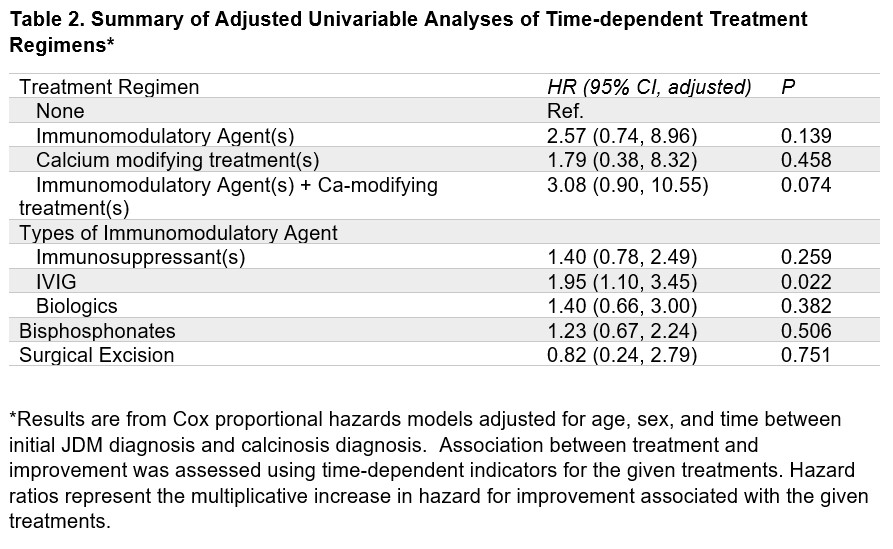
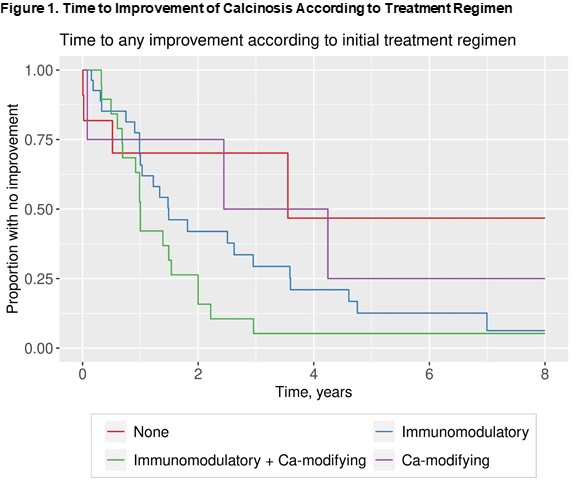
Results: Data for 63 patients were collected from 11 institutions. Median age was 7.8 years at JDM diagnosis with symptom duration occurring for median of 6 months prior, and 9.4 years at calcinosis diagnosis with calcinosis symptoms 2.4 months prior to diagnosis. Calcinosis was present at JDM diagnosis in 32%, and JDM was considered active in 76% of cases at the time of calcinosis diagnosis. Fifty percent of patients had a positive myositis antibody, while 71% had a chronic continuous disease course (Table 1). Seventy nine percent of patients ultimately showed improvement and 22% reached complete resolution. Patients received multiple treatment regimens including immunomodulating agents with or without other calcium modifying treatments (Table 1 footnote). IVIG was associated with greater probability of calcinosis improvement (adjusted HR 1.95; 95% CI 1.10 to 3.45; p=0.02) (Table 2) compared to treatment without IVIG. Patients who received immunomodulatory treatment with other calcium modifying agents tended to show improvement more quickly (Figure 1).
Conclusion: Our study showed that patients with JDM calcinosis received multiple treatment regimens including both immunomodulating therapies and calcium modifying agents, and reassuringly, most patients showed improvement over time. Among the immunomodulating therapies, IVIG was statistically significantly associated with improvement when compared to treatment without IVIG. We plan to study other factors associated with calcinosis outcomes, including analysis of patients with complete resolution. Improved knowledge of treatment choices and outcomes can support future prospective studies.
To cite this abstract in AMA style:
Yi B, Wahezi D, Covert L, Ardalan K, Hui-Yuen J, Vasquez Canizares N, Mosad Mosa D, Jones M, Correll C, Begezda A, Shenoi S, Wu E, Kovalick L, Lapin W, Tarvin S, Oliver M, Rodriguez M, Marmor I, Baszis K, Taxter A, Hanson A, Crowson C, Orandi A. Treatment Response and Outcomes of 63 Cases of Juvenile Dermatomyositis-Associated Calcinosis [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 4). https://acrabstracts.org/abstract/treatment-response-and-outcomes-of-63-cases-of-juvenile-dermatomyositis-associated-calcinosis/. Accessed .« Back to 2023 Pediatric Rheumatology Symposium
ACR Meeting Abstracts - https://acrabstracts.org/abstract/treatment-response-and-outcomes-of-63-cases-of-juvenile-dermatomyositis-associated-calcinosis/