Session Information
Date: Saturday, November 6, 2021
Title: Health Services Research Poster I: Lupus, Inflammatory Arthritis, & More (0128–0148)
Session Type: Poster Session A
Session Time: 8:30AM-10:30AM
Background/Purpose: While recommendations for the treatment of ankylosing spondylitis (AS) are largely aligned across various guidelines,1,2 there remains variability in the treatment. Patients with inflammatory lower back pain, a key symptom of AS, often first visit and receive treatment from their primary care provider (PCP) as opposed to a specialist such as a rheumatologist, which may contribute to this treatment variability. The objective of this analysis was to examine prescribing habits of rheumatologists and PCPs treating AS patients in an academic medical center.
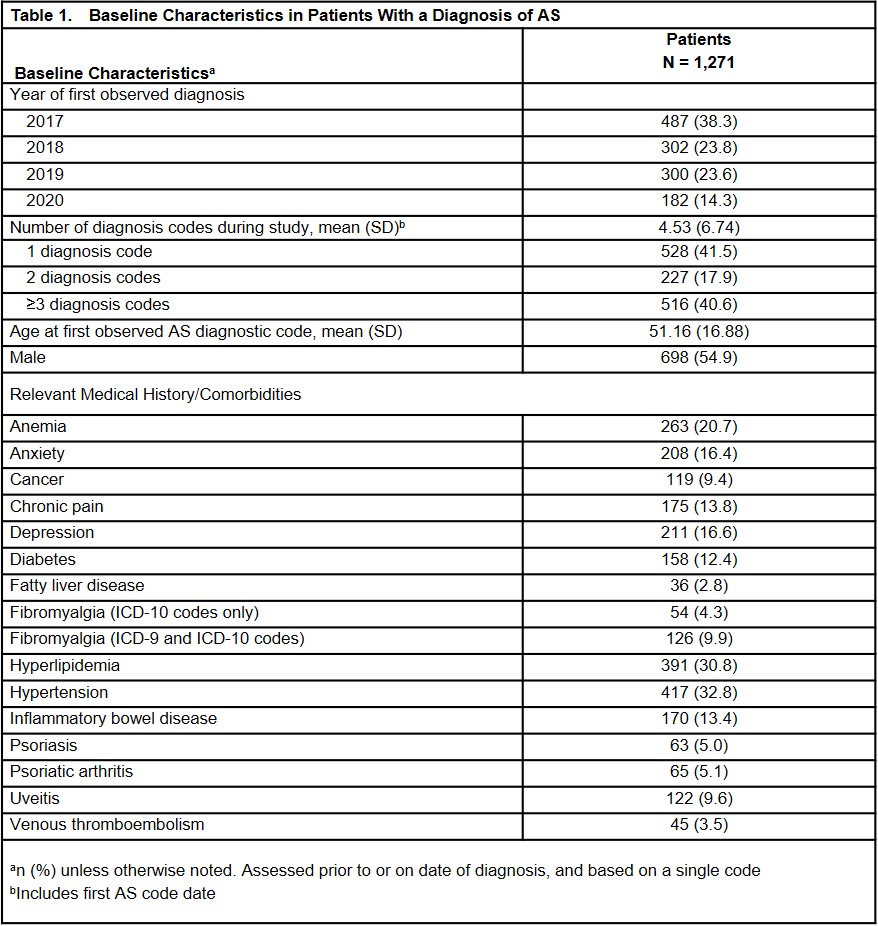
Methods: A retrospective cohort study was performed using the University of Pennsylvania Health System electronic medical record. Patients with a diagnosis of AS (ICD10 M45.X code or M08.1) between January 2017 and September 2020 were included. Baseline characteristics at the time of first diagnosis, visits to rheumatologists and PCPs, and prescribed therapies all within the health system are descriptively reported.
Results: A total of 1,271 patients with a diagnosis code of AS during the study period were identified. The mean age was 51 years, 55% were male, and common comorbidities included hyperlipidemia, hypertension, anemia, and depression (Table 1). Nearly 10% of patients had a diagnosis of uveitis prior to or on the date of the AS diagnosis. Within the healthcare system, 49% of patients were seen by both a rheumatologist and PCP on or after their AS diagnosis; 42% saw only a PCP (Figure 1). Over a third (36%) of patients followed by a rheumatologist were prescribed a biologic disease-modifying antirheumatic drug (bDMARD) during their follow-up, while only 9% of patients followed by a PCP were prescribed a bDMARD (Figure 2). Nearly half of patients followed by only a PCP were prescribed an opiate (49%) or non-opiate (47%) pain medication, while these therapies were prescribed to 16% and 20%, respectively, of patients followed by a rheumatologist without PCP care. Conventional synthetic DMARDs were prescribed to 13% and 5% of patients seen by a rheumatologist only and PCP only, respectively. Among patients followed only by a PCP, opiates (43%), non-opiate pain medication (41%), and NSAIDs (28%) were the most commonly prescribed therapies during the first year after their AS diagnosis. When a patient was followed by both a rheumatologist and PCP, bDMARDs (31%), NSAIDs (27%), and non-opiate pain medications (27%) were most commonly prescribed in the first year.
Conclusion: In this population of patients with AS followed at an academic medical center, bDMARDs and csDMARDs were more frequently prescribed to patients seen by rheumatologists, while opiate and non-opiate pain medications were more frequently prescribed to patients who saw only a PCP. These findings demonstrate the variability in prescribing patterns between PCPs and rheumatologists and highlight areas for targeted education among non-specialists.
References: 1.Ward MM, et al. Arthritis Rheumatol. 2019;71(10):1599-1613.2. van der Heijde D, et al. Ann Rheum Dis. 2017;76(6):978-91.
To cite this abstract in AMA style:
Ogdie-Beatty A, Magrey M, Fitzsimmons R, Abdollahi S, Biljan A, Saffore C, Walsh J. Treatment of Ankylosing Spondylitis by Primary Care Physicians and Rheumatologists in an Academic Health System: A Retrospective Study [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/treatment-of-ankylosing-spondylitis-by-primary-care-physicians-and-rheumatologists-in-an-academic-health-system-a-retrospective-study/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/treatment-of-ankylosing-spondylitis-by-primary-care-physicians-and-rheumatologists-in-an-academic-health-system-a-retrospective-study/