Session Information
Date: Tuesday, November 14, 2023
Title: (1895–1912) Measures & Measurement of Healthcare Quality Poster II
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Treat-to-target (T2T) is a widely established and accepted approach in RA management, but its real-world implementation is suboptimal1. Further primary research is required to identify the most relevant barriers to, and facilitators of, real-world T2T implementation2. This survey assessed perceived barriers to, and facilitators of, T2T implementation among rheumatologists globally.
Methods: A non-remunerated quantitative survey was completed by eligible rheumatologists (≥2 years’ practice experience, awareness of T2T approach, ≥10 patients with RA/year) between June 6 and Sep 30, 2022, in 35 ex-US countries. The survey was informed by a systematic literature review2 and included 9 questions across 6 key areas of T2T implementation in RA: knowledge, skill, confidence, agreement (attitudes/context), contextual/systemic barriers, and behaviors. Knowledge, skill, and confidence were rated on a 5-point scale and reported as suboptimal (no/basic/intermediate knowledge or skill; not/slightly/somewhat confident) or optimal (advanced/expert knowledge or skill; confident/very confident). Agreement was rated on a 6-point scale (strongly disagree to strongly agree) and barriers on a 4-point scale (not at all to serious barrier). Behaviors were rated on a 5-point scale and reported as infrequent (never/rarely/sometimes) or frequent (often/always).
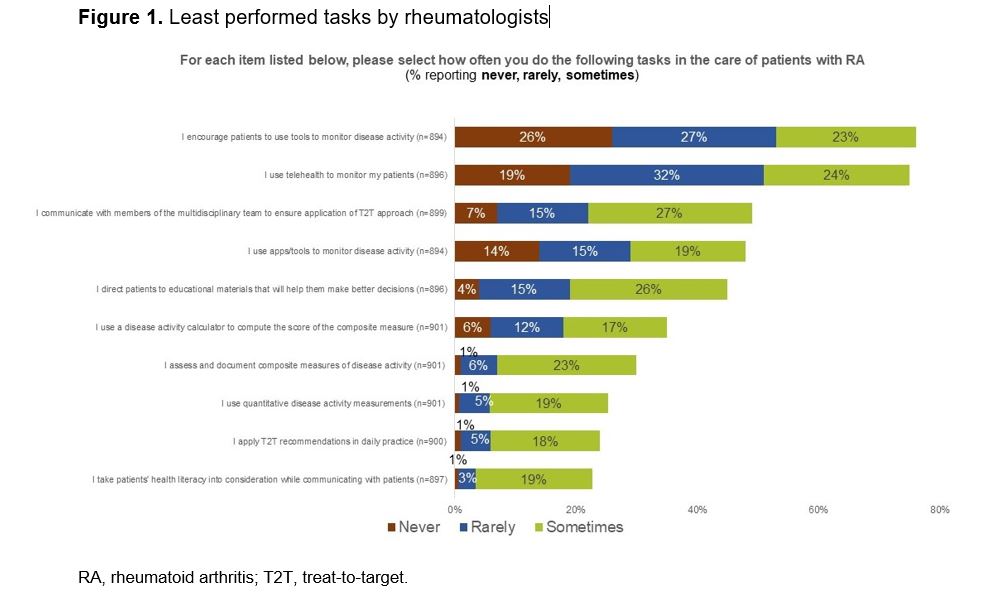
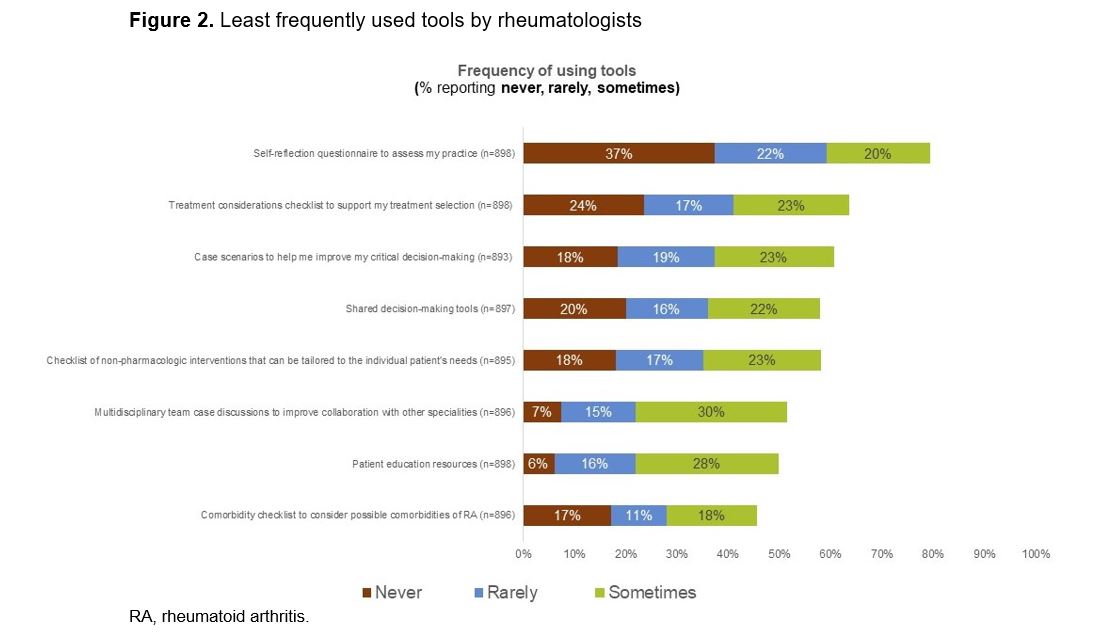
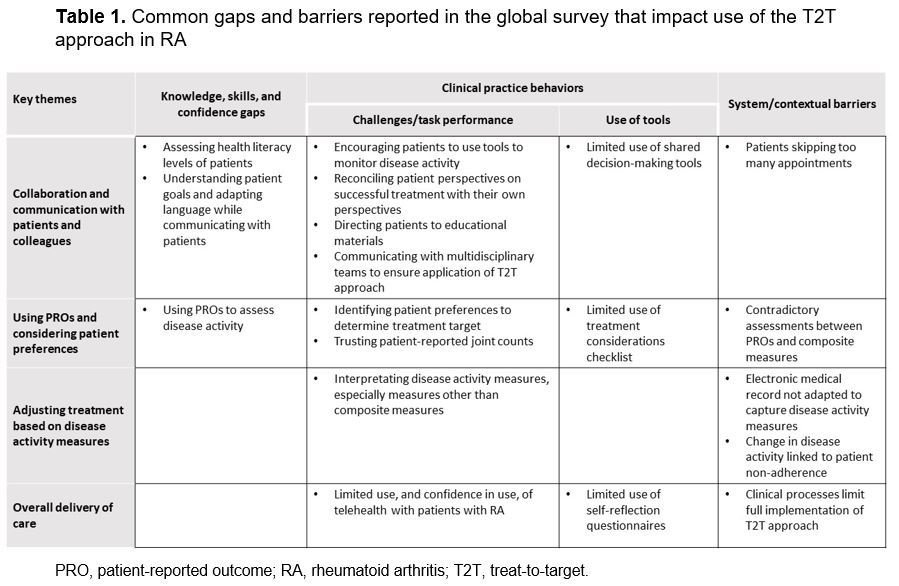
Results: Of 903 surveyed rheumatologists (Europe, n=297; Americas, n=293; Asia-Pacific, n=200; Middle East & Africa, n=113), 72% had ≥11 years of practice experience and 80% reported practicing T2T consistently or frequently. Despite awareness of the T2T approach, there was suboptimal knowledge, skill, and confidence in determining patient health literacy and adapting language while communicating with patients, considering patient goals, and using PROs to assess disease activity. At least 75% of rheumatologists never, rarely, or sometimes used telehealth or encouraged patients to use disease self-assessment tools (Figure 1). The least frequently used tools by rheumatologists were self-reflection questionnaires, treatment considerations checklists, case scenarios, and shared decision-making tools (Figure 2), primarily due to the perception these tools were time-consuming, not needed, or non-existent. Patient adherence-related issues were the top barriers to documenting disease activity, with the other barriers mostly related to healthcare system-related processes. Higher gaps were generally observed in rheumatologists who do not consistently or frequently practice T2T, or who had < 10 years of experience. Table 1 regroups the common gaps and barriers under 4 key themes.
Conclusion: These results highlight practice gaps and educational needs in rheumatologists that can inform educational programs and interventions to support T2T implementation. Based on these findings, recommended focus areas for improving T2T implementation include incorporating all components of T2T in practice, optimal use of telehealth in RA, patient education and shared decision-making, and the use of tools to enhance practice efficiency.
References:
- Yu Z, et al. Arthritis Care Res 2018;70:801–6
- Gossec L, et al. Ann Rheum Dis 2022;81:572 [POS0607]
To cite this abstract in AMA style:
White D, Buch M, Murray S, Caballero D, Nagy O, Takeuchi T. Treat-to-Target in RA Clinical Practice: Global Evidence of Practice Gaps and Educational Needs [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/treat-to-target-in-ra-clinical-practice-global-evidence-of-practice-gaps-and-educational-needs/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/treat-to-target-in-ra-clinical-practice-global-evidence-of-practice-gaps-and-educational-needs/