Session Information
Date: Saturday, November 12, 2022
Title: SLE – Diagnosis, Manifestations, and Outcomes Poster I: Diagnosis
Session Type: Poster Session A
Session Time: 1:00PM-3:00PM
Background/Purpose: Smoking and use of estrogen-containing oral contraceptives (OCP) are SLE risk factors. Data on transitioning from cutaneous lupus erythematosus (CLE) to SLE and potential risk factors associated with that transition remains limited. We aimed to determine the transition rate from CLE to SLE and its associated factors.
Methods: Incident CLE cases were identified based on the modified Gilliam classification scheme in a 27-county region of the American Upper Midwest from 1976-2018. Incident SLE cases were defined according to the European Alliance of Associations for Rheumatology/American College of Rheumatology (EULAR/ACR) criteria. Patients with prior or concurrent SLE diagnosis (SLE diagnosis within 90 days of CLE diagnosis) were excluded. Demographics, BMI, smoking, estrogen-containing OCP use, and CLE subtype were abstracted. CLE patients were followed until SLE diagnosis, death, or emigration out of the 27-county region. Aalen-Johansen methods were used to calculate transition rates from CLE to SLE. Cox-proportional hazards models were used to estimate factors associated with the transition.
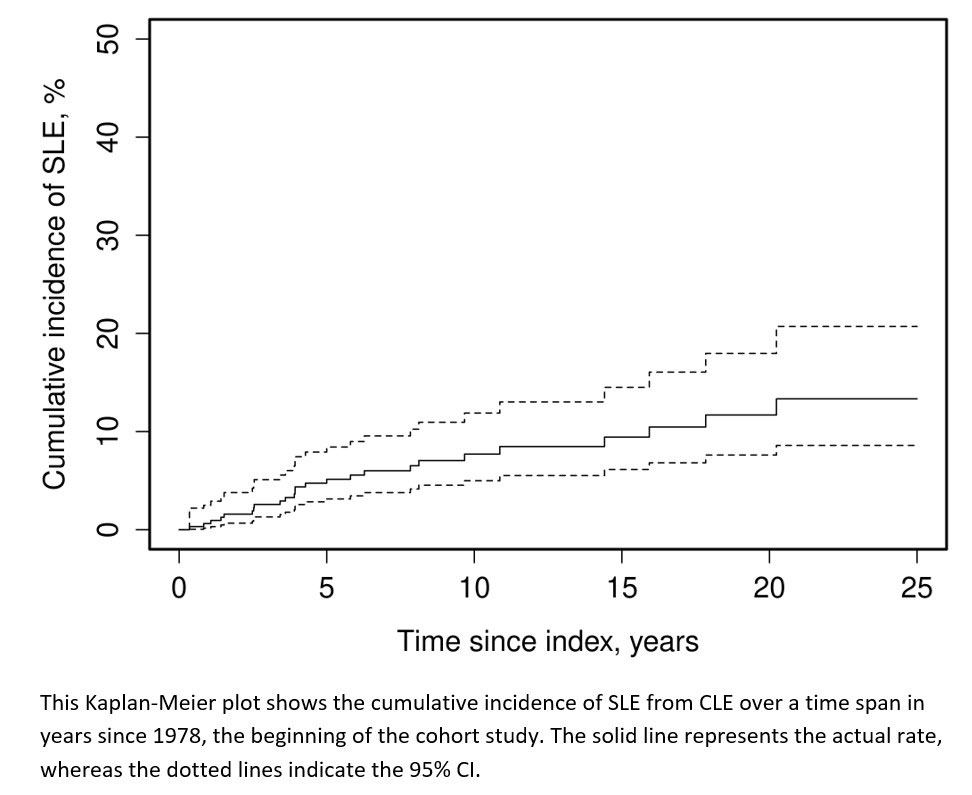
Results: 356 incident CLE cases were identified. 15 were excluded due to the presence of SLE before CLE, and 17 more were excluded due to concurrence of CLE and SLE within 90 days. 324 cases were included in the analysis. During a median follow-up of 8.15 years, 26 patients transitioned to SLE. 20 years after CLE diagnosis 11.8% of CLE patients transitioned to SLE. 5.2% transitioning by 5 years and < 3% transitioning every 5 years from 5-20 years (Figure 1).
Patients with CLE 40 years or younger were more likely to transition to SLE (hazard ratio [HR] 3.25, 95% confidence interval [CI] 1.31 – 8.05) than those older than 50 years. Patients with subacute cutaneous lupus erythematosus (SCLE) were more likely to transition to SLE compared to patients with discoid lupus erythematosus (DLE) (HR 3.6, 95% CI 1.6 – 8.1) and patients with other types of chronic CLE (lupus panniculitis, chilblain lupus or lupus tumidus) (HR 9.3, 95% CI 1.2 – 72.2). Race, sex, family history, calendar year, obesity, smoking, use of estrogen-containing OCPs, and past medical history were not associated with CLE to SLE transition.
Conclusion: The CLE to SLE transition occurred more frequently in patients aged 40 and younger, within the first 10 years of diagnosis, and those with SCLE. Other risk factors studied, including race, sex, family history, calendar year, obesity, smoking, estrogen-containing OCPs, and PMHs, did not affect transitioning.
To cite this abstract in AMA style:
Yang J, Hocaoglu M, Meade-Aguilar J, Sanchez-Rodriguez A, Davis M, Langenfeld H, Crowson C, Duarte-Garcia A. Transitioning from Cutaneous to Systemic Lupus Erythematosus: An Analysis of Incidence and Risk Factors [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/transitioning-from-cutaneous-to-systemic-lupus-erythematosus-an-analysis-of-incidence-and-risk-factors/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/transitioning-from-cutaneous-to-systemic-lupus-erythematosus-an-analysis-of-incidence-and-risk-factors/