Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Myositis-specific autoantibody (MSA) subgroups define phenotypes associated with specific clinical traits and outcomes within JDM, a clinically heterogeneous autoimmune disease. The pathogenesis of JDM is not fully understood. We examined correlation between co-expressed gene modules and clinical traits for JDM and the two top MSA groups (anti-TIF1 and anti-MDA5 autoantibodies (Ab)) to better understand pathogenic differences.
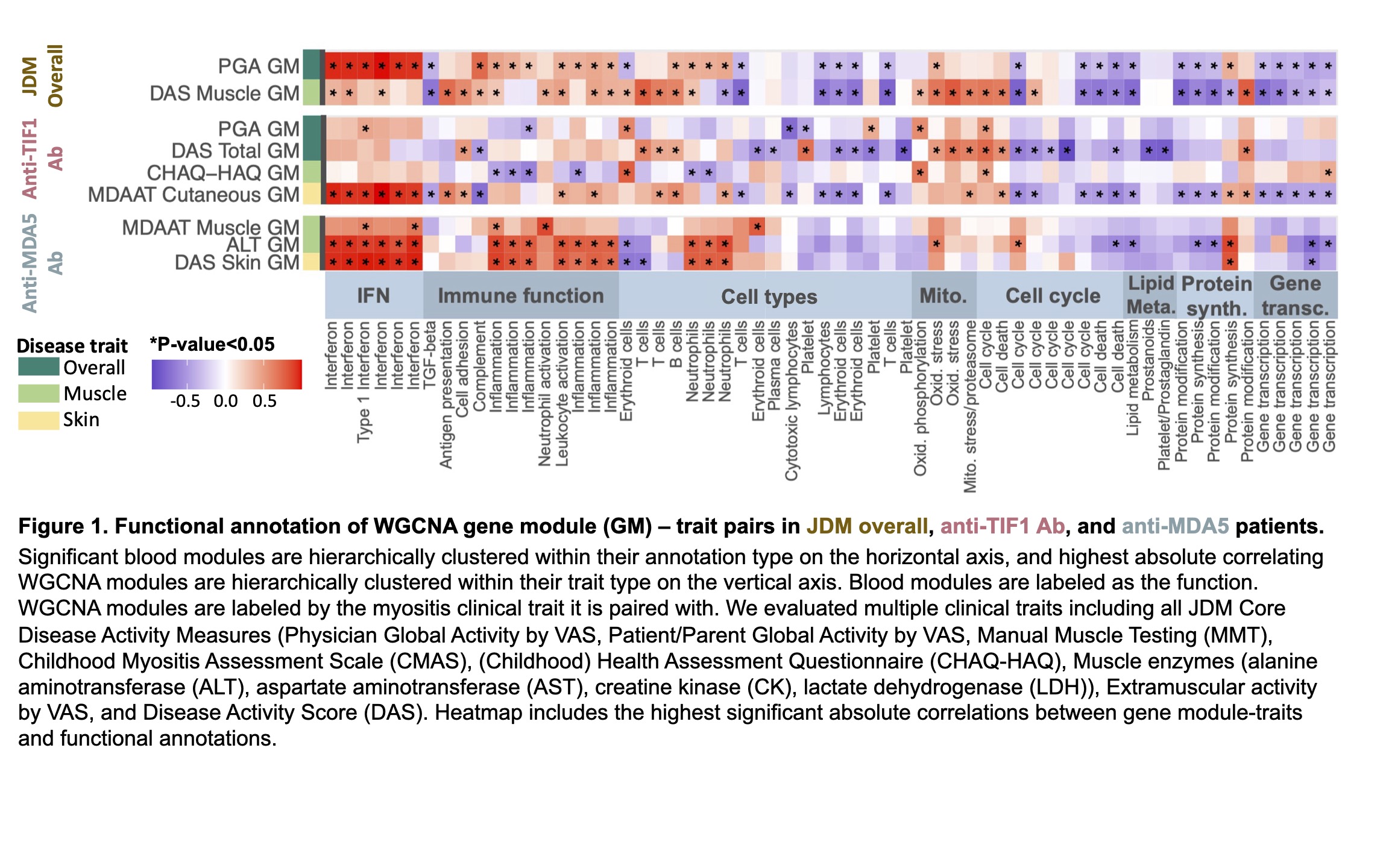
Methods: Whole blood RNA-seq was performed for 56 prevalent JDM patients meeting ACR-EULAR classification criteria with further analysis of the anti-TIF1 (n=22) and anti-MDA5 Ab (n=12) subgroups. Modules of co-expressed genes from weighted gene co-expression network analysis (WGCNA) were correlated with clinical traits. Top-correlating WGCNA-trait pairs were functionally annotated by BloodGen3 modules (Rinchai, 2021). We generated heatmaps of the highest significant absolute Pearson correlations between gene module-traits and functional annotations.
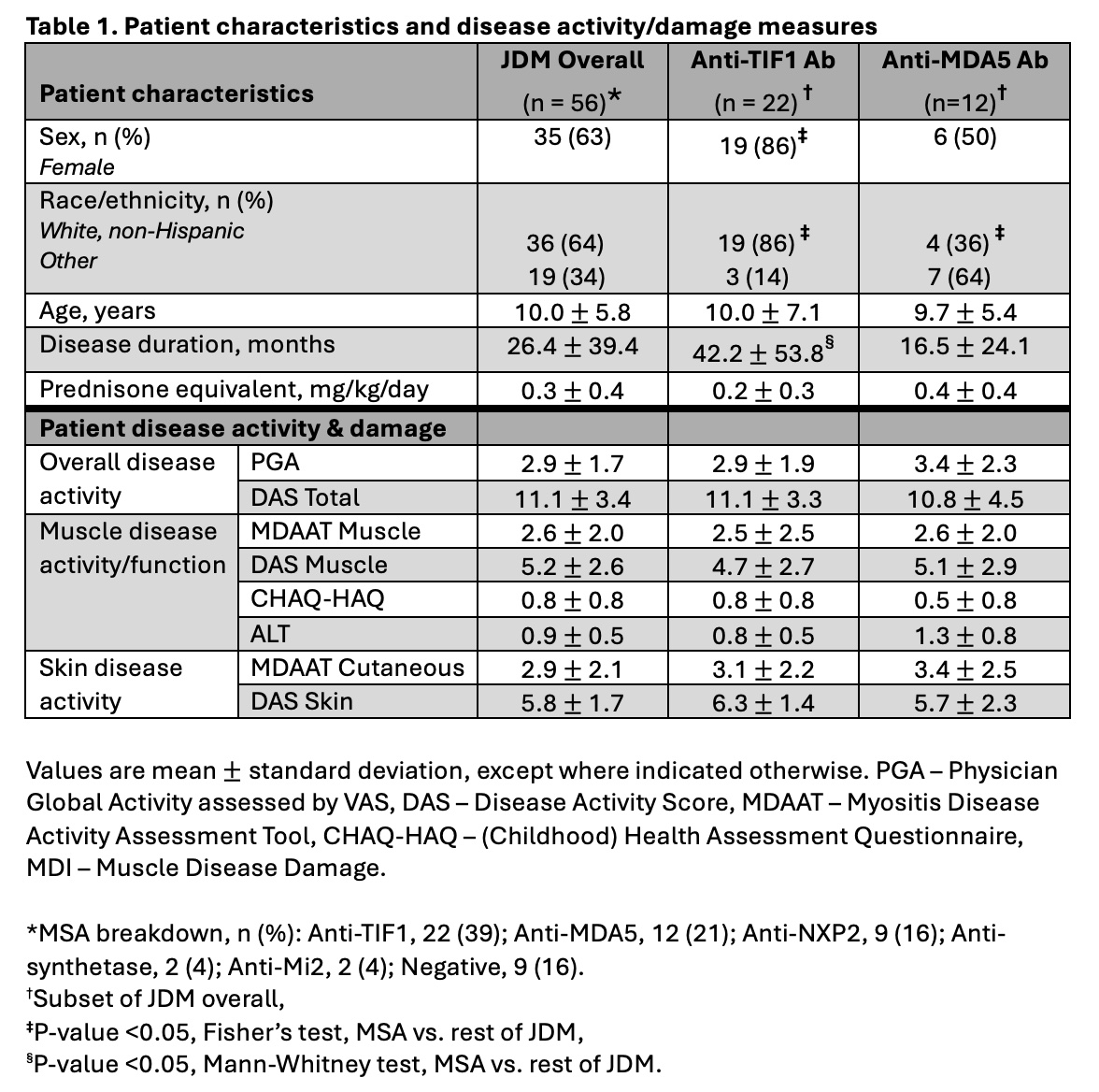
Results: JDM patients were 63% female, 65% white, and averaged 10.0 years old. They had a mean Physician Global Activity (PGA) by Visual Analog Scale score of 2.9/10, an average prednisone dose of 0.3 mg/kg/day, and an average disease duration of 26 months (Table 1). Anti-TIF1 Ab patients had significantly higher proportions of female, non-Hispanic white patients, and longer disease duration versus the rest of JDM patients. Anti-MDA5 Ab patients had a significantly lower proportion of non-Hispanic white patients versus the rest of JDM patients.
In JDM overall patients, overall disease activity (PGA) had high positive correlation with interferon (IFN) (Figure 1). Muscle disease activity had high positive correlations with mitochondrial (oxidative stress), T-cell (cell types), and neutrophil activation (immune function) as well as strong negative correlation with cell cycle.
In anti-TIF1 Ab patients, skin disease activity has highest positive correlation with skin disease activity. Overall disease activity (PGA, Disease Activity Score Total) exhibited strong negative correlation and with cell cycle and platelet (cell type). Function/Muscle disease activity had high positive correlation with erythroid cell, mitochondrial (oxidative phosphorylation), and inflammation (immune category).
In anti-MDA5 Ab patients, both muscle and skin disease activity showed the highest positive correlations to IFN, inflammation, and neutrophil (cell type). Muscle disease activity also strongly correlated positively with neutrophil activation (immune function) and oxidative stress functions.
Conclusion: When comparing groups, IFN functions strongly correlated with overall disease activity in JDM overall, skin disease activity in anti-TIF1 Ab, and both skin and muscle disease activity in anti-MDA5 Ab. Mitochondrial stress functions were found to correlate with muscle disease activity across all groups, while muscle disease activity correlated with neutrophil activation function in JDM overall and anti-MDA5 Ab but not anti-TIF1 Ab. These findings suggest that JDM subgroups may have pathogenic distinctions.
Acknowledgments: Intramural Research Program of the NIH, NIAMS, NIAID, NIEHS, & the CC.
To cite this abstract in AMA style:
Zajmi U, Darrell M, Kaneshiro A, Chin A, Jesus A, Brooks S, Goldbach-Mansky R, Rider L, Kim H. Top Peripheral Blood Transcriptomic Gene Modules Reveal Functional Annotation and Correlation with Clinical Traits in Juvenile Dermatomyositis (JDM) and Myositis-Specific Autoantibody (MSA) Groups [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/top-peripheral-blood-transcriptomic-gene-modules-reveal-functional-annotation-and-correlation-with-clinical-traits-in-juvenile-dermatomyositis-jdm-and-myositis-specific-autoantibody-msa-groups/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/top-peripheral-blood-transcriptomic-gene-modules-reveal-functional-annotation-and-correlation-with-clinical-traits-in-juvenile-dermatomyositis-jdm-and-myositis-specific-autoantibody-msa-groups/