Session Information
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: There are conflicting results about relationship between smoking and incidence of knee osteoarthritis (OA). The effect of smoking to preexisting knee OA has also not been addressed in detail. To address these issues, we designed a retrospective cohort study to investigate the relationship between smoking and knee OA, based on a large-scale claim database from Korea.
Methods: The Korea National Health Insurance Service-Health Screening database is registered with 98% of Koreans and includes all insurance claims. From this database, two retrospective cohort study were conducted. The operational definition of diagnosis of knee osteoarthritis was knee osteoarthritis code (M17) or any site of osteoarthritis code (M15 to M19) along with a knee x-ray (G720, G721). In OA incidence study, the diagnosis of knee osteoarthritis was set as a primary endpoint on OA-naïve people. In OA progression study, we hypothesized that knee replacement surgery is a surrogate marker for progression of knee OA. Thus in OA progression study, the primary endpoint was set as knee replacement surgery (N2072, N2077, N2712, N2717) among previously diagnosed knee OA patients. The study populations were followed from the day of health screening at index year to primary endpoint, the date of death, or December 31, 2019, whichever comes first.
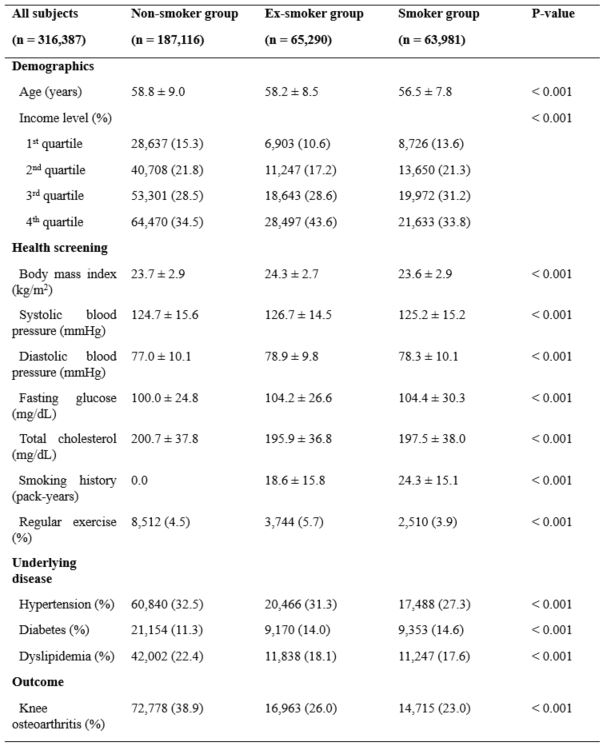
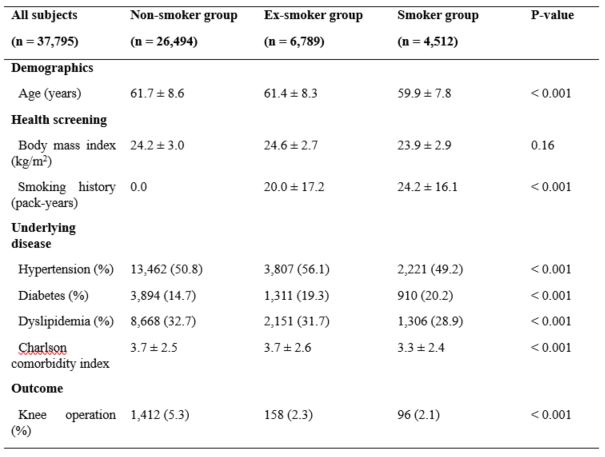
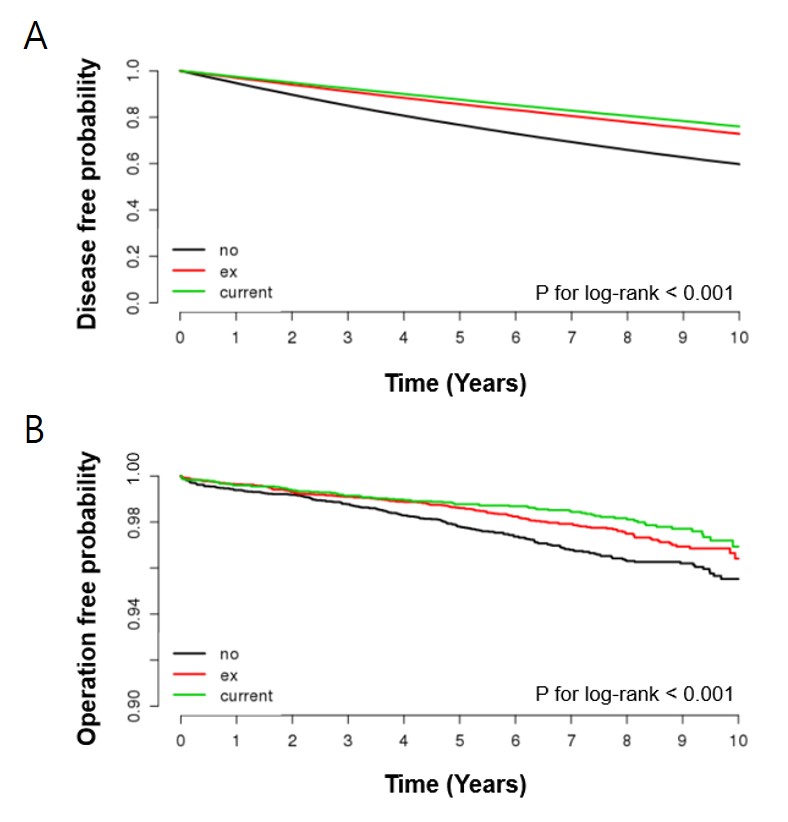
Results: The patient group was classified into non-smoker, ex-smoker, and smoker groups according to the responses to the health examination questionnaire. The baseline characteristics of each group in incidence study and progression study are included in Table 1 and Table 2. The incidence of knee OA was 38.9%, 26%, and 23% in each group of non-smoker, ex-smoker, and smoker group with statistical significance (P-value < 0.001). When the disease-free probability for knee OA was presented using the Kaplan-Meier curve, the risk of knee OA incidence was significantly different between the non-smoker group and the smoker group over time (Figure 1A). The hazard ratio of ex-smoker to non-smoker were 0.95 (0.83-0.97), and those of smoker to non-smoker were 0.89 (0.87-0.91). In knee OA progression study, the frequency of knee replacement surgery due to OA was 5.3% among non-smokers, 2.3% among ex-smokers, and 2.1% among smokers. The Kaplan-Meier curve of knee OA progression study showed that the knee replacement surgery in non-smoker group was more frequent than ex-smoker group and non-smoker group as time passed (Figure 1B). The adjusted hazard ratio of ex-smoker to non-smoker were 0.81 (0.66-0.99, p=0.04) and those of smoker to non-smoker were 0.76 (0.61-0.96, p=0.02).
Conclusion: This large-scale retrospective cohort study revealed that both incidence and frequency of knee replacement surgery, one of the indicators of progression of knee osteoarthritis, was lower in smoker group and ex-smoker group than in non-smoker group. Further studies on exact mechanism of smoking and osteoarthritis are required.
To cite this abstract in AMA style:
Park J, Son M, Lee S, Chung W, Lee S. Tobacco Smoking Reduces the Incidence and Delays the Progression of Knee Osteoarthritis: 10-year Retrospective Cohort Study Based on Korea National Health Insurance Service-Health Screening Database [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/tobacco-smoking-reduces-the-incidence-and-delays-the-progression-of-knee-osteoarthritis-10-year-retrospective-cohort-study-based-on-korea-national-health-insurance-service-health-screening-database/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/tobacco-smoking-reduces-the-incidence-and-delays-the-progression-of-knee-osteoarthritis-10-year-retrospective-cohort-study-based-on-korea-national-health-insurance-service-health-screening-database/