Session Information
Session Type: ACR Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Interstitial lung disease (ILD) is a significant contributor to rheumatoid arthritis (RA) mortality, yet its pathogenesis remains enigmatic. One theory posits that initial inflammatory RA-ILD pathology occurs secondary to systemic inflammation, prior to transitioning to irreversible fibrotic lung disease. This idea is supported by the TNF-transgenic (TNF-Tg) mouse model of RA, which manifests a purely inflammatory pulmonary pathology of interstitial infiltrate, perivascular inflammation, vascular occlusion, and follicle formation. While anti-TNF agents are largely effective for arthritis, some reports have found them to be ineffective, and possibly detrimental, to patients with RA-ILD. Here, we tested the hypothesis that pre-fibrotic inflammatory ILD is reversible by treating established ILD in TNF-Tg mice.
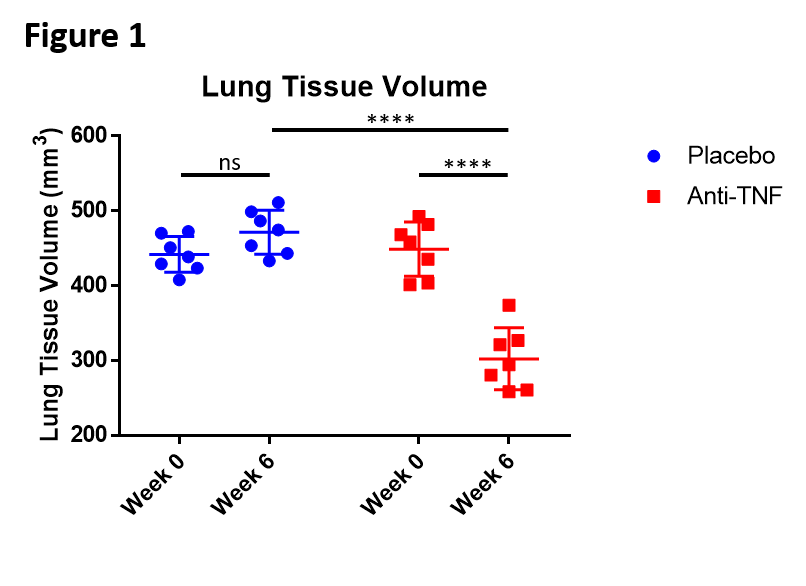
Methods: TNF-Tg mice underwent in vivo micro-computed tomography (µCT) to establish baseline ILD. Once they achieved a minimum lung tissue volume of 400mm3, mice (n=6) were randomized to 6-weeks of treatment with anti-TNF or Placebo (10mg/kg/wk i.p.). Body weight, grip strength, and knee ultrasound were measured bi-weekly. Terminal outcomes included lung µCT, histology, and flow cytometry.
Results: Anti-TNF treated mice recovered their body weight, grip strength and had resolution of their arthritis. Further, they demonstrated a dramatic yet incomplete amelioration of lung pathology. Total lung tissue volume was significantly reduced vs. placebo (302.25 +/- 38.40mm3 vs. 471.53 +/- 27.13mm3; p<0.0001) (Fig. 1). Histologic analysis corroborated this finding, with marked decreases in interstitial infiltrate, perivascular inflammation, and vascular occlusion in anti-TNF treated lungs. In contrast, prominent follicle-like structures remained (Fig. 2A-C). Flow cytometry identified a novel CD11bint/CD11c– population, which declined with a concomitant increase in a CD11bhi/CD11chi cDC2-like population in placebo treated lungs, and reverted to WT in the anti-TNF treated lungs (Fig. 2D-F).
Conclusion: Our results demonstrate that a purely inflammatory RA-ILD is largely resolved with anti-TNF therapy, supporting the hypothesis that the inflammatory phase of ILD is potentially reversible. Interestingly, the follicle-like structures in the pulmonary tissue were not cleared by anti-TNF therapy, and a novel cell population was identified in TNF-Tg mice lungs that was no longer present after anti-TNF therapy. Further research is needed to investigate the role of the follicle-like structures and to characterize this novel cell population.
To cite this abstract in AMA style:
Wu E, Bell R, Schwarz E, Rahimi H. TNF-α Blockade Incompletely Reverses Inflammatory Pulmonary Pathology in the TNF-Transgenic Mouse Model of Rheumatoid Arthritis [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/tnf-%ce%b1-blockade-incompletely-reverses-inflammatory-pulmonary-pathology-in-the-tnf-transgenic-mouse-model-of-rheumatoid-arthritis/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/tnf-%ce%b1-blockade-incompletely-reverses-inflammatory-pulmonary-pathology-in-the-tnf-transgenic-mouse-model-of-rheumatoid-arthritis/