Session Information
Date: Tuesday, October 28, 2025
Title: (1830–1854) Systemic Lupus Erythematosus – Etiology and Pathogenesis Poster
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Patients with systemic lupus erythematosus (SLE) face elevated risk of thrombotic events (TEs) due to traditional cardiovascular factors and chronic inflammation. Statins may offer anti-inflammatory effects beyond lipid lowering, making them potentially valuable in this population. This retrospective cohort study examines the association between statin use and TEs in SLE patients, aiming to clarify inconsistent findings in prior research and optimize further management strategies.
Methods: We conducted a retrospective cohort study using the Mount Sinai Health System’s Epic-linked electronic medical record to identify patients >18 years old diagnosed with SLE via ICD-10 codes between January 2000 and March 2024. Patients not meeting the 2019 ACR/EULAR classification criteria for SLE were excluded. The primary outcome of the study was the occurrence of a TE (arterial or venous), assessed using time to event analysis from the time of SLE diagnosis to the TE event or last follow-up. Patients free of a TE by the time of the last follow-up were censored. Statin use was the primary predictor variable. Univariate extended Cox models were utilized to explore the role of seven independent variables, including the primary exposure of interest as a time-dependent variable, on the risk of thrombotic events. P-values < 0.05 were considered statistically significant.
Results: A total of 376 patients with SLE were included in the study. Patient demographics, hydroxychloroquine use, as well as concomitant comorbidities of smoking, hypertension, diabetes mellitus, secondary antiphospholipid syndrome (APS) and lupus nephritis are detailed in Table 1. Of the 376 patients, 6.4% experienced thrombotic events during follow-up; 35.6% of these patients had a diagnosis of secondary APS. In univariate analyses, statin use, and secondary antiphospholipid syndrome (APS) showed significant associations with TEs. However, due to sparse data and wide confidence intervals, particularly among patients without APS, APS variable was excluded from the final model. Statin exposure was unexpectedly associated with an increased hazard of thrombotic events (HR 6.62; 95% CI: 2.44–17.93; p < 0.001; Table 2, Table 3).
Conclusion: While these results were statistically significant, the wide confidence interval suggests variability in the estimate, likely reflecting the limited number of events among non-statin users and heterogeneous exposure timing. These findings should be interpreted in the context of an exploratory analysis and warrant further investigation in a larger study. Results likely also reflect residual confounding, such as the preferential use of statins in higher-risk patients. Similar findings have been reported in other chronic inflammatory conditions, suggesting that statins alone do not sufficiently address thrombotic risk in people living with SLE.
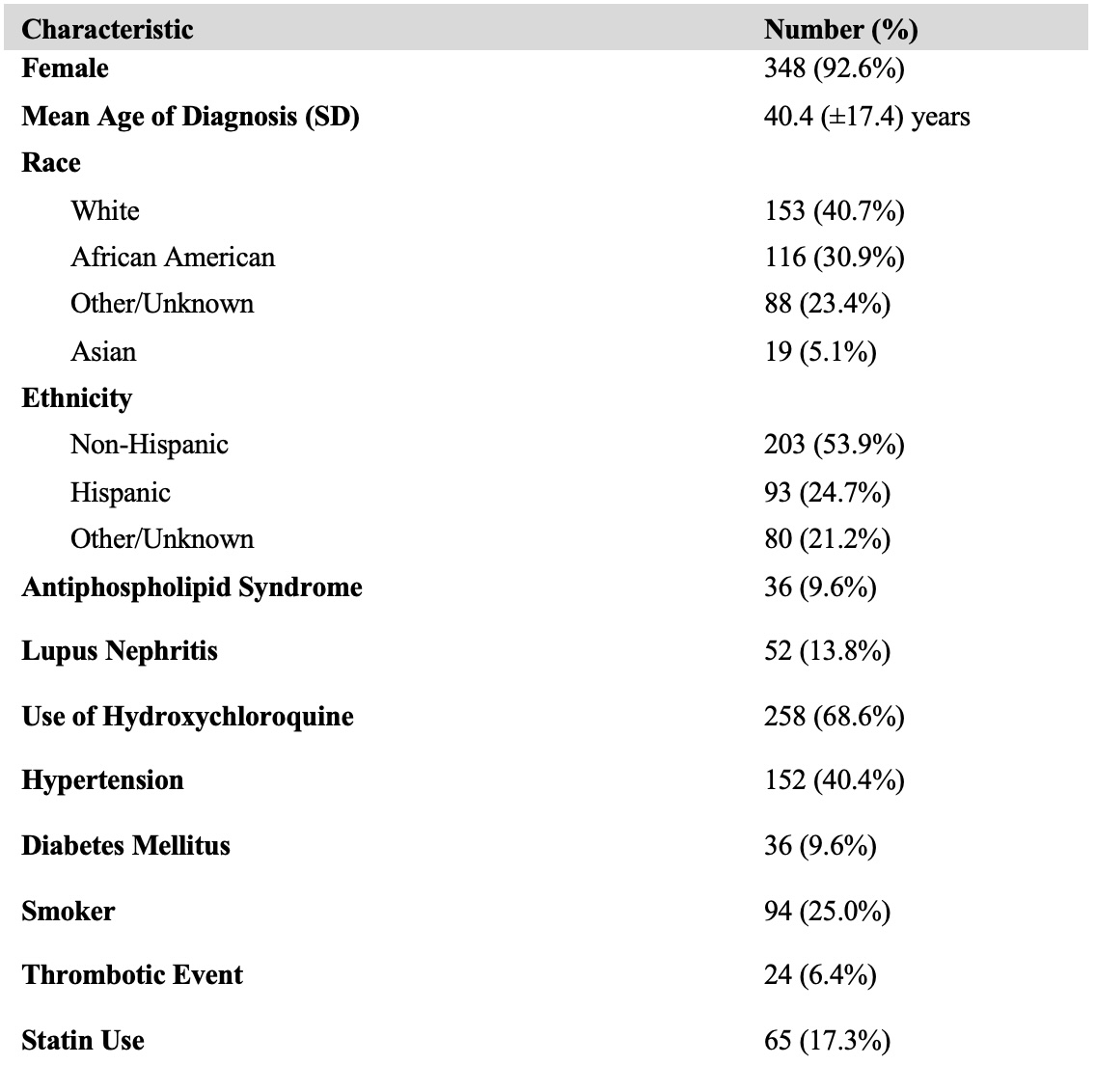 Table 1. Patient clinical characteristics and co-morbidities.
Table 1. Patient clinical characteristics and co-morbidities.
.jpg) Table 2. Univariate extended Cox models of thrombotic risk by demographics, comorbidities, and treatment variables.
Table 2. Univariate extended Cox models of thrombotic risk by demographics, comorbidities, and treatment variables.
.jpg) Table 3. Final extended Cox model assessing the association between time-dependent statin use and thrombotic events.
Table 3. Final extended Cox model assessing the association between time-dependent statin use and thrombotic events.
To cite this abstract in AMA style:
Lenchur C, Liranzo Tejera N, Abonamah A, Matsui T, Cosentino E, Abate Namnum P, Marushchak O, Akselrad M, John M, Lutgen S, He C, Oladeinde B, Sidhu H, Bagiella E, Wright I, Dobrowolski C. Time-to-Event Analysis of Statin Use and Thrombotic Risk in Patients with Systemic Lupus Erythematosus: A Single-Center Retrospective Study [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/time-to-event-analysis-of-statin-use-and-thrombotic-risk-in-patients-with-systemic-lupus-erythematosus-a-single-center-retrospective-study/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/time-to-event-analysis-of-statin-use-and-thrombotic-risk-in-patients-with-systemic-lupus-erythematosus-a-single-center-retrospective-study/
