Session Information
Date: Wednesday, November 15, 2023
Title: Abstracts: Miscellaneous Rheumatic & Inflammatory Diseases III
Session Type: Abstract Session
Session Time: 9:00AM-10:30AM
Background/Purpose: VEXAS (vacuoles, E1 enzyme, X-linked, autoinflammatory, somatic) syndrome, due to somatic mutations in the UBA1 gene, is an autoinflammatory disorder associated with an increased thrombotic risk. We investigated the frequency and characteristics of thrombotic events in patients with VEXAS syndrome, as well as their impact on survival.
Methods: This retrospective, multi-center study utilized electronic medical records from the National Institutes of Health (NIH) Clinical Center and Mayo Clinic, along with referred outside records, to identify patients with VEXAS syndrome who had a confirmed UBA1 somatic mutation and VEXAS clinical features. The time of symptom onset was used as the time of disease onset. Thrombosis was considered VEXAS disease onset if it occurred within two years of inflammatory symptom onset. SVT was excluded as a thrombotic event for analysis. Univariate and multivariate logistic regression analysis was used to identify predictors of thrombosis. Kaplan-Meier curve models were applied to estimate overall survival (OS). Statistical significance was P < .05. Lupus anticoagulant (LA) was assessed in 41 patients and other coagulation assays in 27.
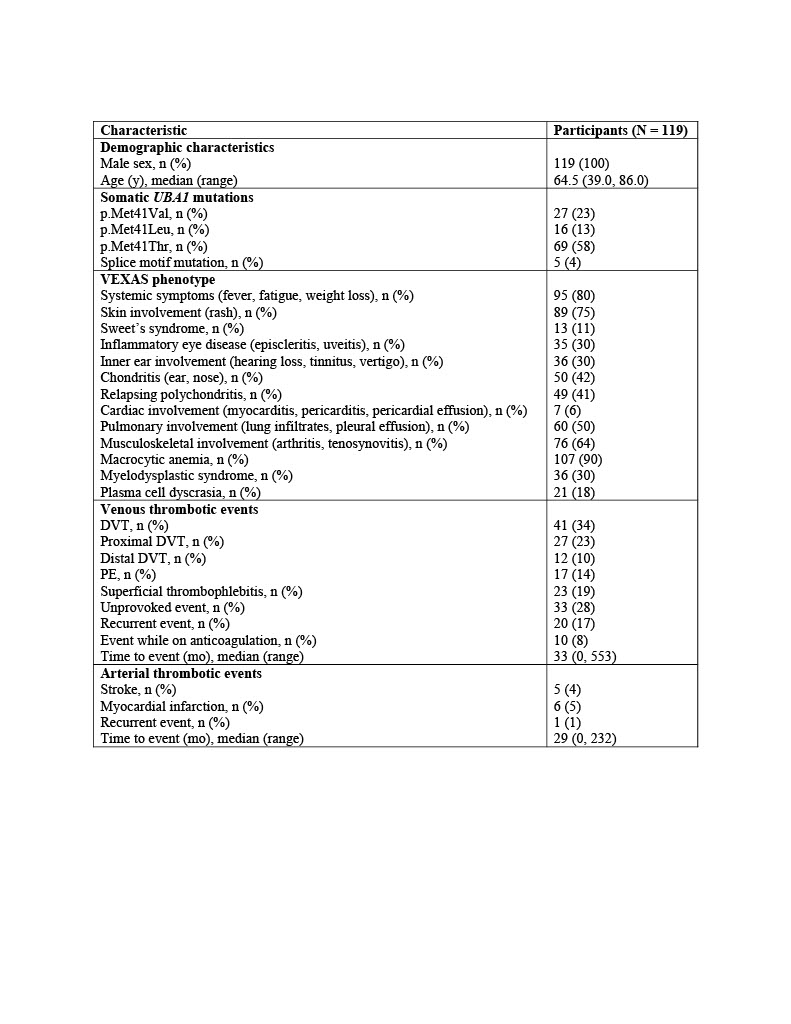
Results: A total of 119 VEXAS patients were included. All patients (100%) were male with a median age of 65 years (39-86 years). Hematologic manifestations included macrocytic anemia in 107 (90%), myelodysplastic syndrome (MDS) in 36 (30%), and plasma cell dyscrasia (PCD) in 21 (18%).
Of the 119 patients, 58/119 (49%) had a thrombotic event. Of those, 51 (43%) had VTE, and 9 (8%) had arterial events (AT), with a median time from disease onset of 33 and 29 months, respectively; seven patients (6%) had both venous and AT. The majority of VTE events were unprovoked 33 (28%) and over one-third 20 (17%) were recurrent, and 10 (8%) on anticoagulation (Table 1).
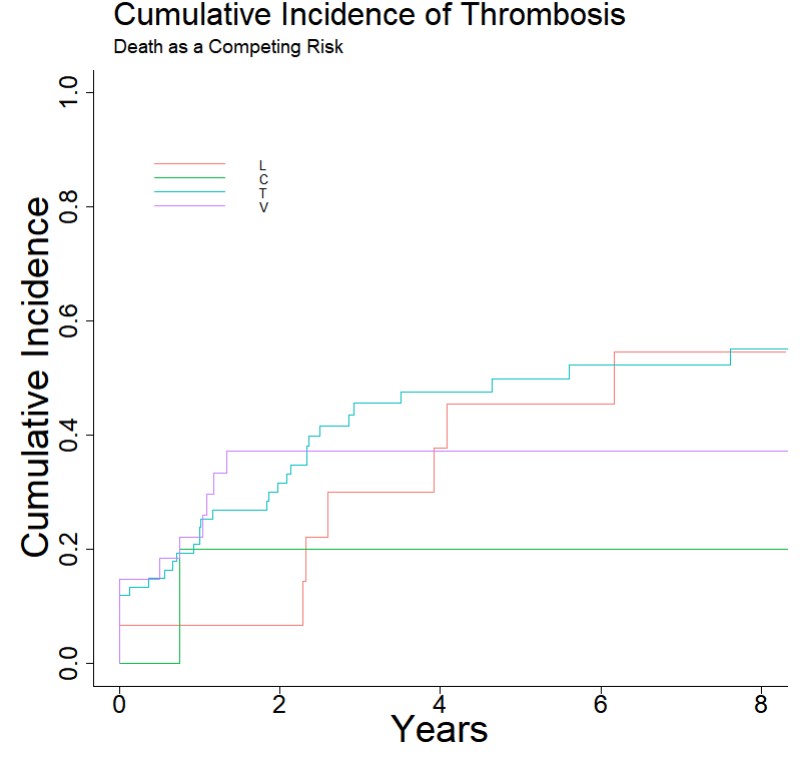
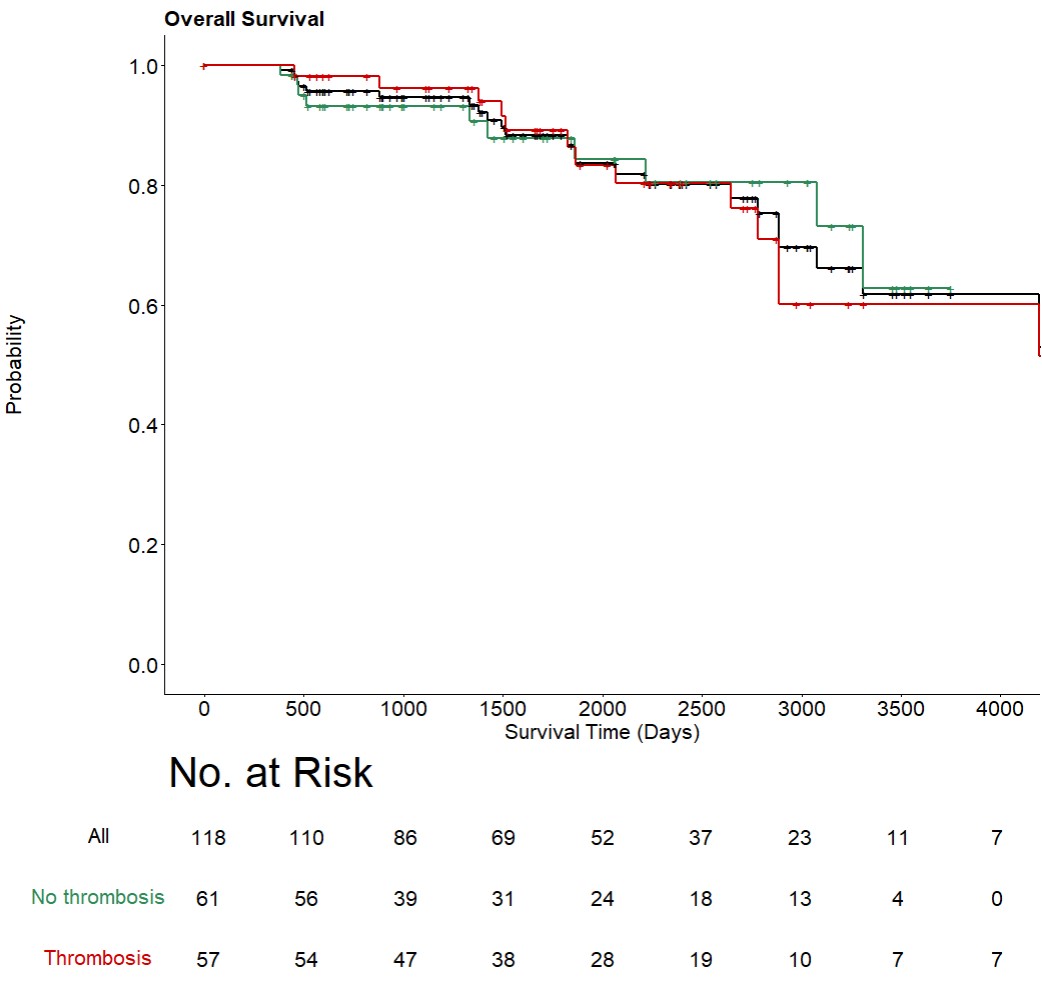
The cumulative incidence (CI) at a median follow-up of DVT, PE, and arterial thrombosis was 28.7%, 9.7%, and 8.7% respectively. CI at median follow-up of any thrombotic event was 22% for UBA1 M41L, 40% for M41T, and 37% for M41V, however, rising CI was seen with M41L over time while occurring early in M41T and M41V (Figure 1). The M41L UBA1 variant was positively associated with PE in univariate (OR: 4.58; p=0.02) and multivariate (OR: 16.94; p = 0.01) analyses but not with DVT or arterial thrombosis. The median OS from disease onset was 1740 days with no significant difference in OS between patients with (86.9%) or without (89.7%) thrombosis (Figure 2). In the univariate and multivariate Cox proportional hazard model, thrombosis was not associated with worse OS. The majority of VEXAS patients had high factor VIII levels (26/27; 96%) and VWF activity (16/27; 59%), while most had high VWF antigen (11/25; 44%), factor IX levels (12/27; 44%) and protein C activity (11/27; 41%). CRP and ESR were positively correlated with D-dimer and negatively correlated with VWF activity. LA was positive in 16/41 (40%) and correlated significantly with higher CRP (p< 0.01).
Conclusion: Patients with VEXAS syndrome are at high risk of VTE, which can recur despite anticoagulation therapy. Considering the high prevalence of thrombosis in VEXAS patients, it is crucial to assess their VTE risk carefully and consider prophylactic anticoagulation.
To cite this abstract in AMA style:
Ghorbanzadeh A, Kusne Y, Dulau-Florea A, Shalhoub R, Alcedo P, Nghiem K, Ferrada M, hines a, Panicker S, ombrello a, Reichard K, Darden I, Goodspeed W, wilson L, Olteanu H, Lasho T, Kastner D, Warrington K, Mangaonkar A, Go R, Beck D, Patnaik M, Young N, Calvo K, Casanegra A, Grayson P, Koster M, Wu C, Houghton D, Patel B, Kanthi Y, Groarke E. Thrombosis in Patients with VEXAS Syndrome: A Retrospective Cohort Study [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/thrombosis-in-patients-with-vexas-syndrome-a-retrospective-cohort-study/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/thrombosis-in-patients-with-vexas-syndrome-a-retrospective-cohort-study/