Session Information
Session Type: Poster Session D
Session Time: 8:30AM-10:30AM
Background/Purpose: Management and outcomes of multisystem inflammatory syndrome in children (MIS-C) remain under investigation and vary by institution. This study aimed to describe the outcomes of MIS-C patients treated at our center, and compare these outcomes based on initial management.
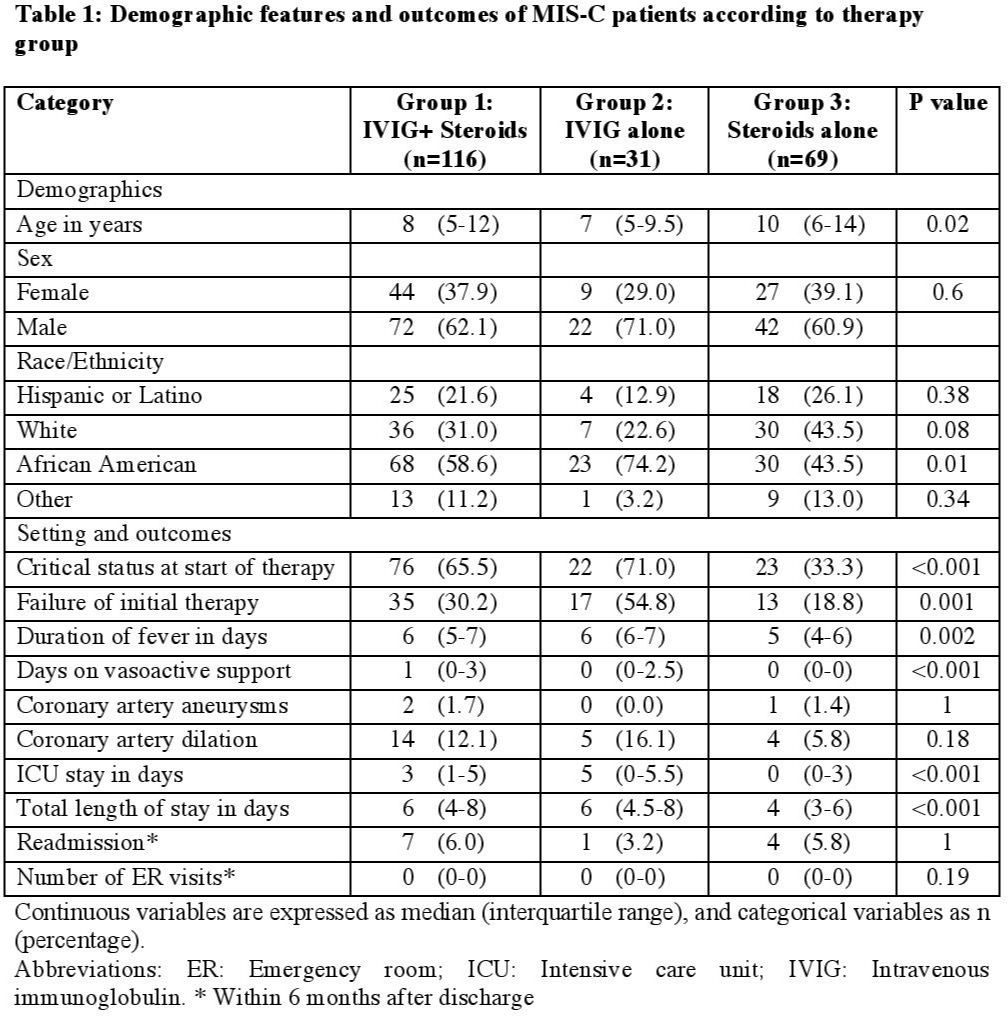
Methods: A single center retrospective study was conducted; all patients with MIS-C diagnosis between March 2020 and February 2021 were eligible. Demographic and clinical variables were collected. Patients were divided into 3 groups, based on immunomodulation within the first 24 hours of treatment initiation for patients in the intensive care unit (ICU), or 48 hours for non-ICU patients. The primary outcome was failure of initial therapy defined as need to escalate immunosuppression due to fever, worsening laboratory parameters, and/or lack of improvement/worsening cardiac or non-cardiac findings. Secondary outcomes included duration of fever and vasoactive support, coronary aneurysms/dilation, length of ICU stay, hospital length of stay, readmission, and number of emergency room (ER) visits up to 6 months after discharge. Groups were compared using Kruskal Wallis test for continuous variables and Fisher/Chi-square test for categorical variables, employing R software. P values of ≤0.05 were considered statistically significant.
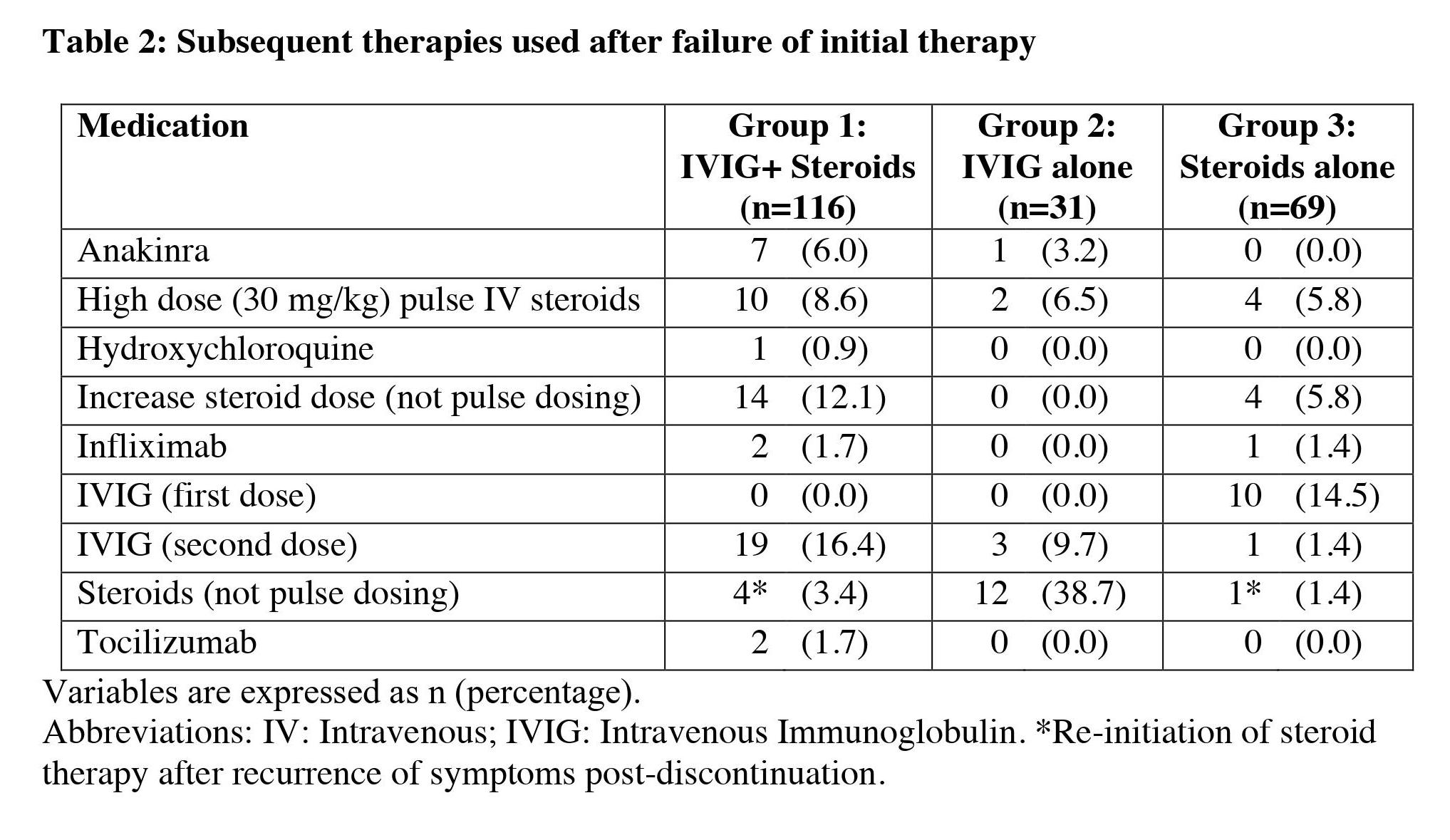
Results: Two-hundred and thirty-one MIS-C patients were identified. Patients who did not receive immunomodulation (n=5), required biologics within the first 24 hours (n=3), received intravenous immunoglobulin (IVIG) at another center (n=3), or received therapy escalation without meeting the definition of failure of initial therapy (n=4) were excluded. Of the remaining 216 subjects, 116 received IVIG + steroids (Group 1), 31 received IVIG alone (Group 2), and 69 received steroids alone (Group 3) as initial therapy. Maximum initial steroid dose was methylprednisolone/prednisone 2 mg/kg/day. The groups differed in age and racial distribution; patients in group 3 were older (p = 0.02) and less frequently of African American race (p = 0.01). ICU status at the start of therapy was less frequent in group 3 (33.3%) vs group 1 (65.5%) and 2 (71%) (p < 0.001). Rates of initial therapy failure were lowest in group 3 (18.8% vs 30.2% and 54.8% for groups 1 and 2, respectively; p = 0.001). Group 3 had shorter duration of fever (median 5 days vs 6 days in group 1 and 2; p = 0.002), ICU length of stay (median 0 days vs 3 and 5 days for group 1 and 2, respectively; p < 0.001), and total length of stay (median 4 days vs 6 days in groups 1 and 2; p < 0.001). Vasoactive support duration was longer for group 1 (median 1 day vs 0 days for groups 2 and 3; p < 0.001). Coronary outcomes, need for readmission and ER visits post-discharge were similar between groups. All patients survived.
Conclusion: A subgroup of MIS-C patients was successfully treated with steroid monotherapy. This group was older, less frequently African American, likely had milder disease (less frequent ICU status), had lower rates of treatment failure and favorable secondary outcomes. For a subset of MIS-C patients, steroid monotherapy could be a suitable alternative to IVIG. Multivariate analysis controlling for severity and prospective studies are needed to further explore these findings.
To cite this abstract in AMA style:
Villacis Nunez D, Jones K, Fan L, Moore W, Jabbar A, Oster M, Jaggi P, Prahalad S. Therapy Based Outcomes in Patients with Multisystem Inflammatory Syndrome in Children: A Single Center Study [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/therapy-based-outcomes-in-patients-with-multisystem-inflammatory-syndrome-in-children-a-single-center-study/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/therapy-based-outcomes-in-patients-with-multisystem-inflammatory-syndrome-in-children-a-single-center-study/