Session Information
Session Type: Abstract Session
Session Time: 1:00PM-2:30PM
Background/Purpose: Women with SLE have high rates of preeclampsia caused by poor placental vascularization. The FDA recently approved the ratio of two angiogenic factors, soluble fms-like tyrosine kinase 1 (s-Flt1) and placental growth factor (PlGF), as a diagnostic test for preeclampsia. In women without rheumatic disease, over 90% have an sFlt1:PlGF ratio ≤ 38. An sFlt1:PlGF ratio this low rules out preeclampsia, while an sFlt1:PlGF ratio > 85 is predictive of preeclampsia. We sought to determine whether these thresholds could rule-out or rule-in preeclampsia in women with SLE.
Methods: Pregnancies came from a prospective registry and met these criteria: entry ≤30 weeks gestation, serum sample ≥20 weeks gestation, and singleton. Preeclampsia, including post-partum preeclampsia, was determined by a roundtable of six experts. All laboratory measurements occurred at routine rheumatology visits. We tested if a low sFlt1:PlGF ratio (≤38) was associated with the absence of preeclampsia at 4- and 8- weeks post-draw, and during the entire pregnancy/postpartum, and if a high sFlt1:PlGF ratio ( >85) was associated with preeclampsia at the same time points. We assessed pregnancies overall, and stratified by urine protein: creatinine ratio at the time of the visit (UPCR >300 vs. ≤300 mg/g).
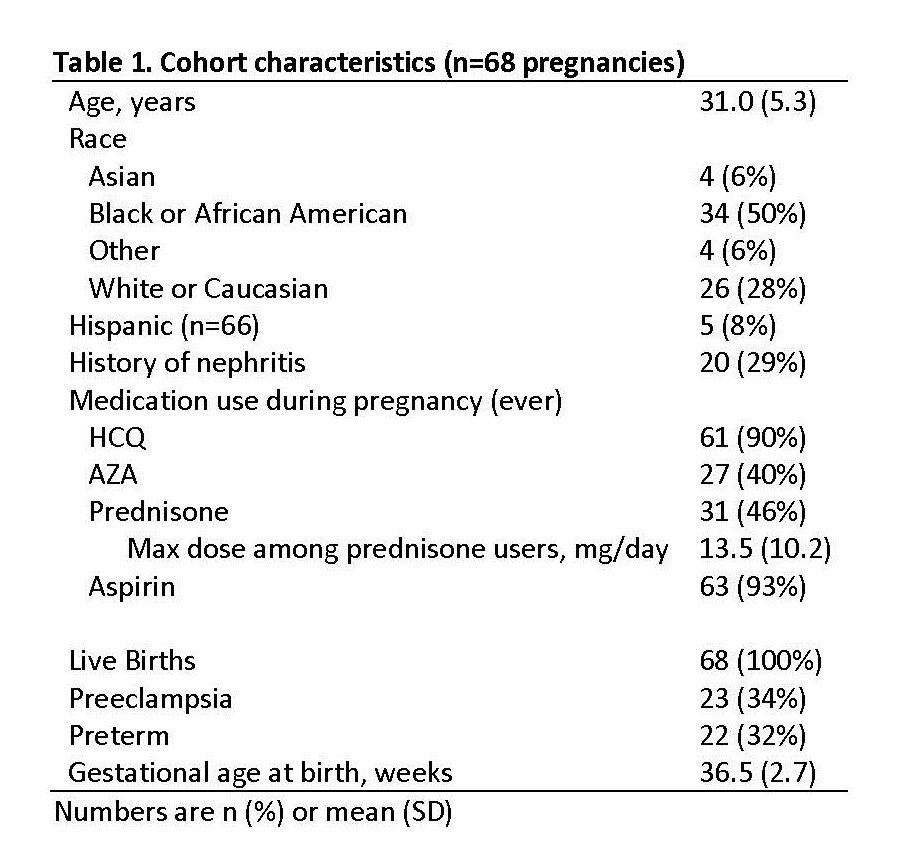
Results: The cohort included 107 samples from 68 women with SLE, 29% with a history of lupus nephritis and 16% with active nephritis during pregnancy (per SLEPDAI renal definitions) (Table 1). Average maternal age was 31; 50% of women self-identified as Black and 38% as White. Preeclampsia incidence was 34% and the majority of test results (62%) had an sFlt1:PlGF ratio >38.
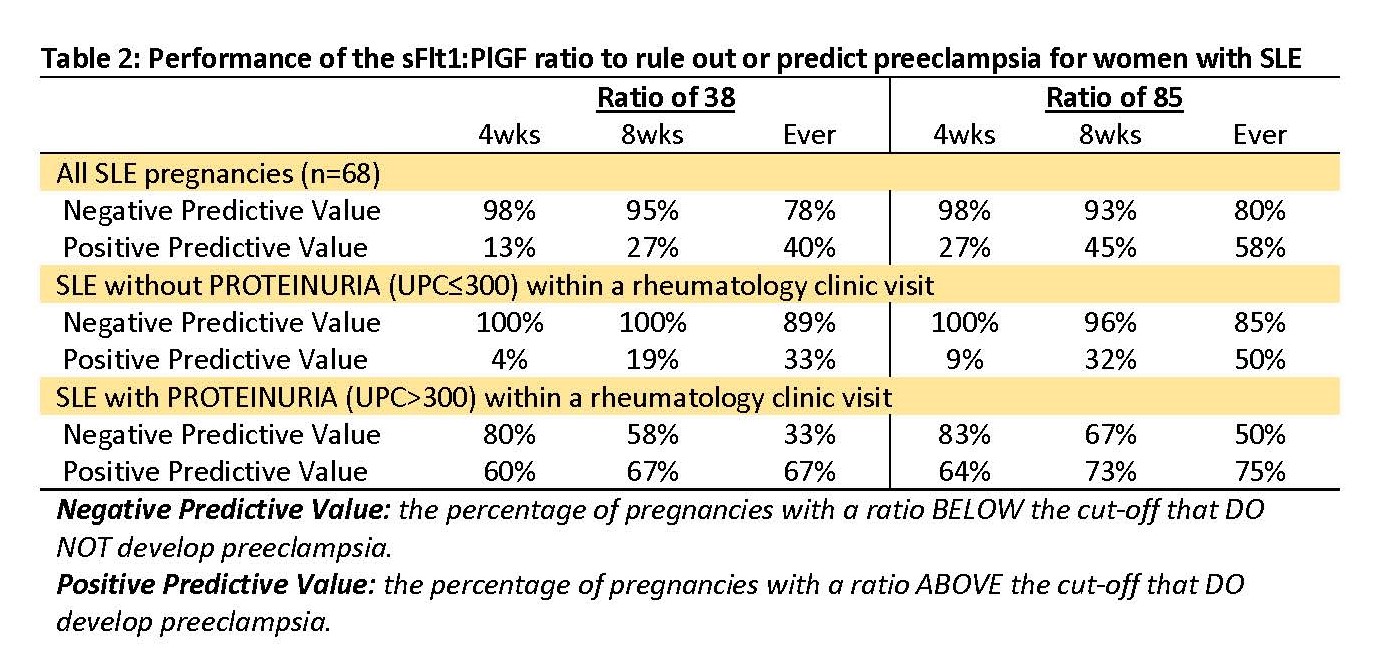
All SLE pregnancies: Pregnancies with sFlt1:PlGF≤38 were unlikely to develop preeclampsia (Table 2). sFlt1:PlGF>85 was modestly effective in predicting preeclampsia.
Pregnancies without proteinuria: Both sFlt1:PlGF≤38 and sFlt1:PlGF≤85 very effectively ruled out preeclampsia (NPV >95% within 8 weeks). sFlt1:PlGF>38 was not predictive of preeclampsia. Of the 14 patients who developed preeclampsia without having proteinuria in the clinic visit, 12 had sFlt1:PlGF>38 (sensitivity 86%). sFlt1:PlGF>85 was not predictive of preeclampsia within 4-weeks, but a third developed preeclampsia within 8-weeks and half had preeclampsia eventually.
Pregnancies with proteinuria: sFlt1:PlGF≤38 largely ruled out preeclampsia within the next 4 weeks (NPV 80%), but two-thirds eventually had preeclampsia. sFlt1:PlGF>38 was moderately predictive of preeclampsia and sFlt1:PlGF>85 was more predictive of preeclampsia.
Conclusion:
The high frequency of an elevated sFlt1:PlGF ratio among women with SLE highlights poor placental vascularization with SLE. Having neither proteinuria nor a high sFlt1:PlGF effectively ruled out preeclampsia. Having either proteinuria or a high sFlt1:PlGF suggested preeclampsia was unlikely within the next 4 weeks, but these patients were at high risk for subsequent preeclampsia. Having both proteinuria and a high sFlt1:PlGF ratio made preeclampsia likely to occur. The cut-off of sFlt1:PlGF≤38 effectively rules out preeclampsia for women with SLE without proteinuria; for those with proteinuria, a low sFlt1:PlGF≤38 suggests preeclampsia is not imminent.
To cite this abstract in AMA style:
Clowse M, Addae-Konadu K, Federspiel J, Gilner J, James A, Kovalik E, Lucas A, Neil L, Sims C, Snyderman A, Soneji S, Eudy A. The Utility of the sFlt1:PlGF Ratio to Rule out and Predict Preeclampsia in Women with Lupus [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/the-utility-of-the-sflt1plgf-ratio-to-rule-out-and-predict-preeclampsia-in-women-with-lupus/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-utility-of-the-sflt1plgf-ratio-to-rule-out-and-predict-preeclampsia-in-women-with-lupus/