Session Information
Date: Sunday, November 7, 2021
Title: Epidemiology & Public Health Poster II: Inflammatory Arthritis – RA, SpA, & Gout (0560–0593)
Session Type: Poster Session B
Session Time: 8:30AM-10:30AM
Background/Purpose: Rheumatoid arthritis (RA) carries a substantial burden for patients and society in terms of morbidity, disability, and medical expenses. The Australian Pharmaceutical Benefits Scheme (PBS) subsidised biological disease-modifying anti-rheumatic drugs (bDMARD) since 2003. We investigated the association between subsidised bDMARD therapy for RA in 2003 hospitalisation rates and health care costs.
Methods: Hospital admissions for RA patients between 1995 and 2014 were identified in the Western Australia (WA) Hospital Morbidity Data Collection (ICD codes 714 and M05.00–M06.99). State-specific dispensing data for conventional DMARD (cDMARD) and bDMARD for RA was obtained from Statistics Australia and expressed as defined daily doses /1000 population/day (DDD) using the WA population census. Principal component analysis (PCA) was applied to determine the relationship between DMARD use and hospital admission rates. Total expenditure for DMARD and RA hospital admissions were obtained from the PBS domain and Australia’s health care expenditure report.
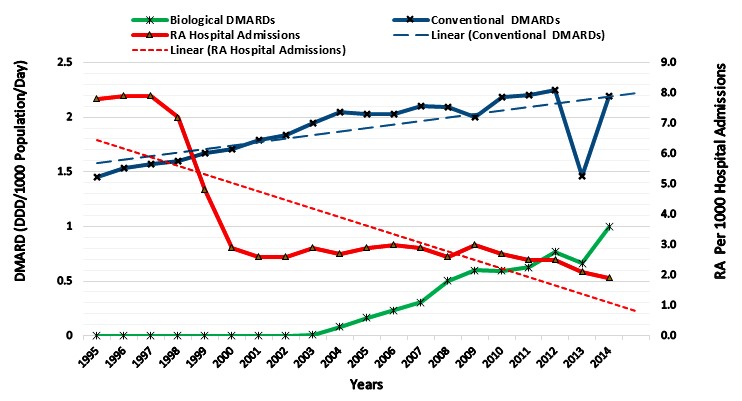
Results: A total of 17,125 patients had 50,353 admissions with a diagnostic code for RA. Between 1995 and 2002, the number of RA admissions fell from 7.9 to 2.6/1,000 admissions, while cDMARD use rose from 1.45 to 1.84 DDD. Between 2003–2014, RA admissions decreased further to 1.9/1,000 hospital admissions, while cDMARD use increased to 2.19 DDD and bDMARDs from 0.01 to 1.0 DDD. In PCA analysis, cDMARD (methotrexate and leflunomide) and bDMARD use had an inverse relationship with hospital admission rates. The annual costs of bDMARD utilisation was 22.5 million in 2003–2014, while annual cost savings of RA hospital admissions was 9.2 million.
Conclusion: The increased use of cDMARD use for RA has coincided with a significant decline in hospital admissions for RA patients in WA, while a more modest further decline followed bDMARD introduction. BDMARD therapy was not as cost-effective as cDMARD in relation to RA hospital admissions costs.
To cite this abstract in AMA style:
Almutairi K, Nossent J, Preen D, Keen H, Inderjeeth C. The Temporal Association Between Hospital Admissions, Disease-modifying Anti-rheumatic Drugs Usage and Direct Health Care Costs in Rheumatoid Arthritis Patients [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/the-temporal-association-between-hospital-admissions-disease-modifying-anti-rheumatic-drugs-usage-and-direct-health-care-costs-in-rheumatoid-arthritis-patients/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-temporal-association-between-hospital-admissions-disease-modifying-anti-rheumatic-drugs-usage-and-direct-health-care-costs-in-rheumatoid-arthritis-patients/