Session Information
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Vasculitis of the peripheral nervous system is seen mainly in systemic vasculitis involving small and medium sized vessels and in cases of single-organ vasculitis affecting the peripheral nerves. There are no pathognomonic tests to confirm a diagnosis of vasculitis other than histopathological findings of vasculitis affecting the vasa nervorum. However, the diagnostic yield of biopsies from affected peripheral nerves and the correlation of pathological confirmation with clinical features is largely unknown. The aims of this study were to (i) characterize patients undergoing sural nerve biopsy in the search of vasculitis, (ii) estimate the diagnostic yield, (iii) correlate biopsy findings with demographic, laboratory and clinical parameters, (iv) estimate the rate of surgical complications and (v) to study possible predictors of a positive biopsy.
Methods: A retrospective cohort study was conducted at Skåne University Hospital (Sweden) and Addenbrooke’s Hospital (Cambridge, United Kingdom). Patients that underwent sural nerve biopsy between 2005 and 2019 in the region of Skåne were identified by search in the regional pathology database and by search on the surgical procedure code in the clinical register. Patients that underwent sural nerve biopsy between 2015-2019 at Addenbrooke’s Hospital were identified by search in the local pathology database. A structured review of the medical case records and pathology reports was performed. Patients with a suspected vasculitis were included in the study. Histopathologic biopsy findings were recorded as definite, probable or non-vasculitis in accordance with validated guidelines. Definite and probable histopathologic biopsy findings were regarded as a positive biopsy. Surgical complications were recorded when available in the medical case record.
Results: Out of 94 identified patients, vasculitis was diagnosed in 40 (43%) patients based on findings in the sural nerve biopsy (definite =14, probable =26). (Table 1) A positive biopsy finding was associated with ANCA-positivity (p=0.029), a higher white blood cell count (p=0.007) and organ involvement other than from the nervous system at the time of the biopsy (p=0.039). A positive biopsy finding was associated with a longer median length of the biopsy sample (p=0.042). The biopsy sample length was 30 mm (IQR: 18-42.5) and 21 mm (IQR: 14-33) for positive and negative biopsies respectively. (Table 2) However, no parameter was shown to be an independent predictor of a positive biopsy after a multivariate adjustment of the regression model. Post-surgical follow-up was available in 60 patients with a reported sural nerve surgical complication rate of 17%. The most common presentations were wound infection (10%), wound dehiscence (7%), and delayed wound healing (5%). A concomitant muscle biopsy was performed in 11 patients. None of the muscle biopsies added to the diagnostic yield. (Table 1)
Conclusion: Sural nerve biopsy is a useful and safe procedure to confirm a diagnosis of vasculitis especially in patients with a systemic involvement and positive ANCA. In this study, a combined nerve and muscle biopsy did not add to the diagnostic yield.
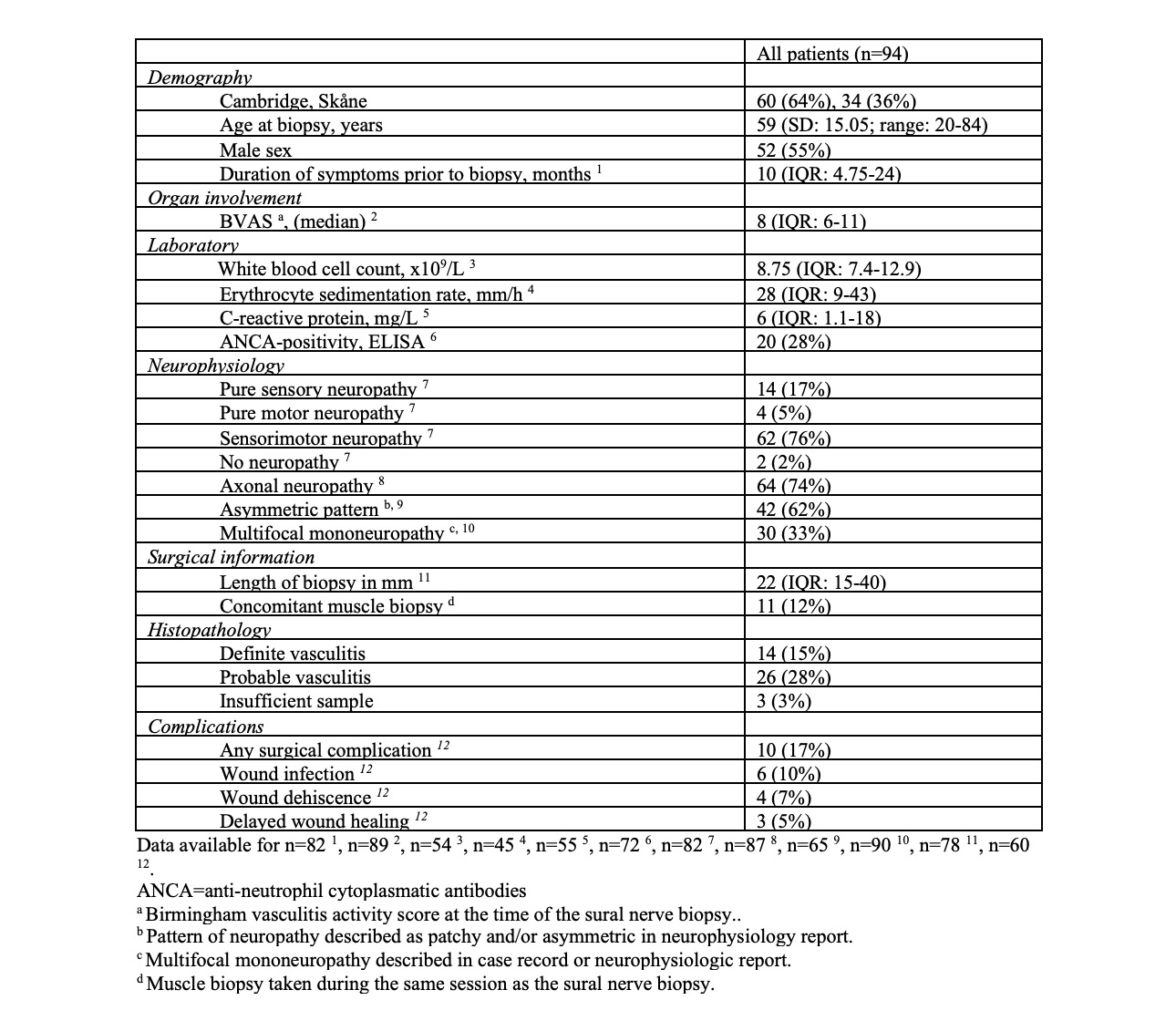 Table 1. Cohort characteristics
Table 1. Cohort characteristics
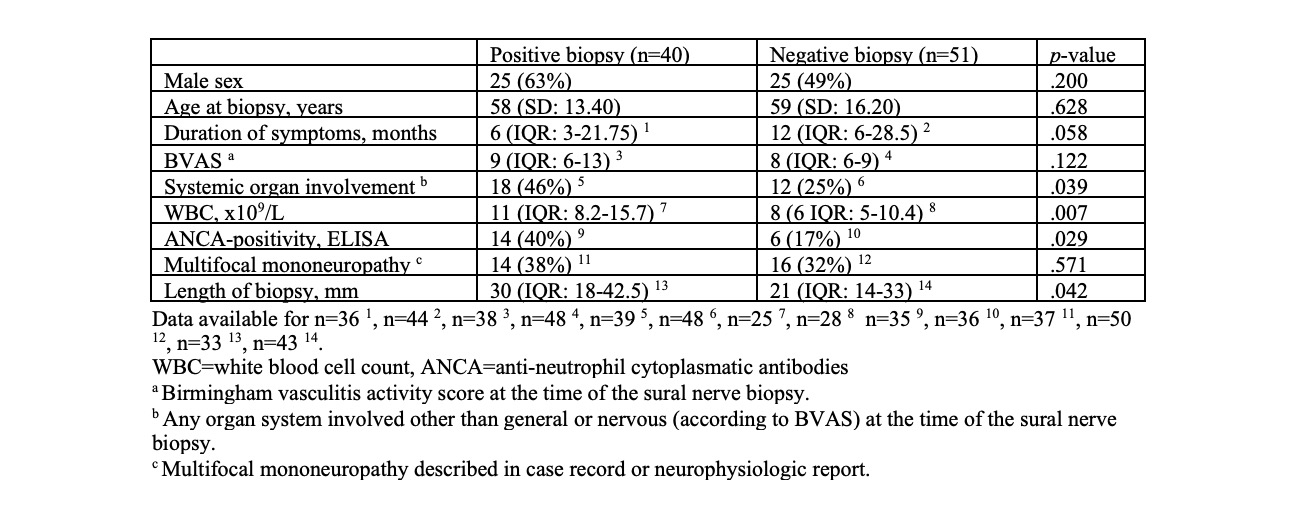 Table 2. Features in patients with positive vs. negative sural nerve biopsy (excluding patients with insufficient biopsy)
Table 2. Features in patients with positive vs. negative sural nerve biopsy (excluding patients with insufficient biopsy)
To cite this abstract in AMA style:
Gisslander K, Dahlin L, Smith R, Jayne D, Mohammad A. The Role of Sural Nerve Biopsy in the Diagnosis of Systemic Vasculitis – a Retrospective Study from Two Specialized Centres [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/the-role-of-sural-nerve-biopsy-in-the-diagnosis-of-systemic-vasculitis-a-retrospective-study-from-two-specialized-centres/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-role-of-sural-nerve-biopsy-in-the-diagnosis-of-systemic-vasculitis-a-retrospective-study-from-two-specialized-centres/
