Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Systemic sclerosis (SSc) manifests through a diverse interplay of inflammatory, fibrotic, and vascular alterations, intricately entwined in its pathogenesis, which encompasses immune system dysregulation, tissue fibrosis, and vascular dysfunction. While elevated C-reactive protein (CRP) levels in SSc have been associated with the early inflammatory phases of the disease, comprehensive data regarding the influence of CRP on SSc activity and severity remain limited. This study aims to investigate the significance of inflammatory phenotypes in clinical parameters among individuals with SSc and to assess the prognostic importance of baseline and persistent inflammatory phenotypes in SSc.
Methods: A cross-sectional study involving 133 SSc patients meeting the 2013 ACR/EULAR criteria was conducted. Patients were categorized into inflammatory (CRP≥ 5 mg/l) and non-inflammatory (CRP< 5mg/l) phenotypes at the first visit and additionally stratified into persistent inflammatory/non- inflammatory phenotypes (CRP≥ 5 mg/l for more than 80% of visits). Cox regression models analysed mortality risk and ILD development. Logistic regression assessed the risk of major organ involvement (ILD, PH,
scleroderma renal crisis, heart involvement, peripheral vasculature involvement) relative to inflammation at SSc onset, adjusting for conceptual confounders.
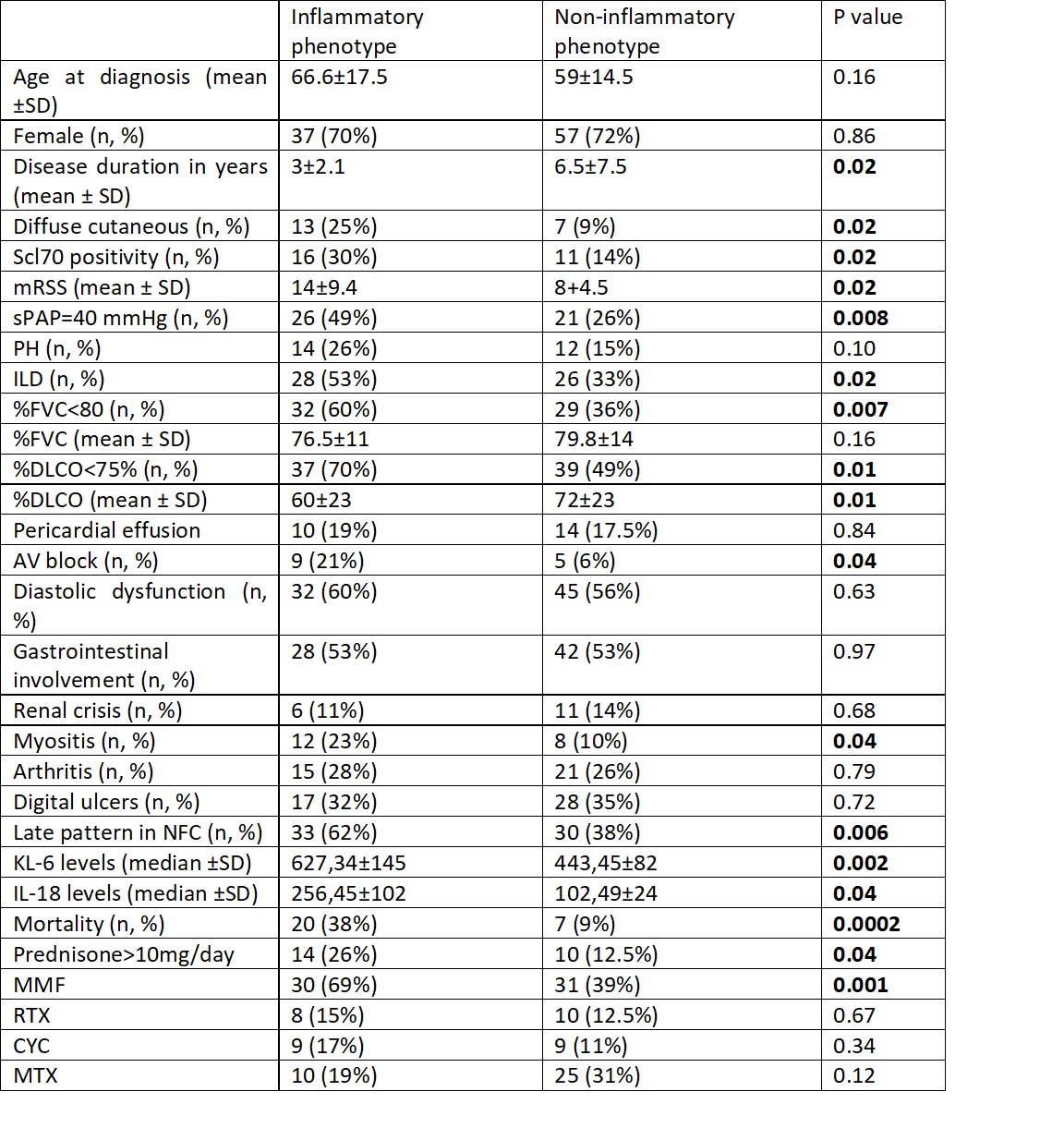
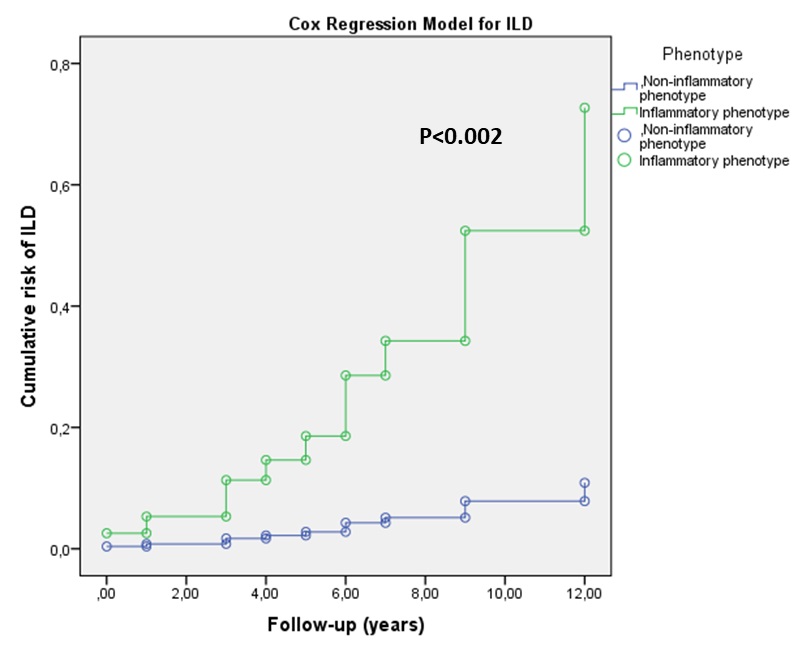
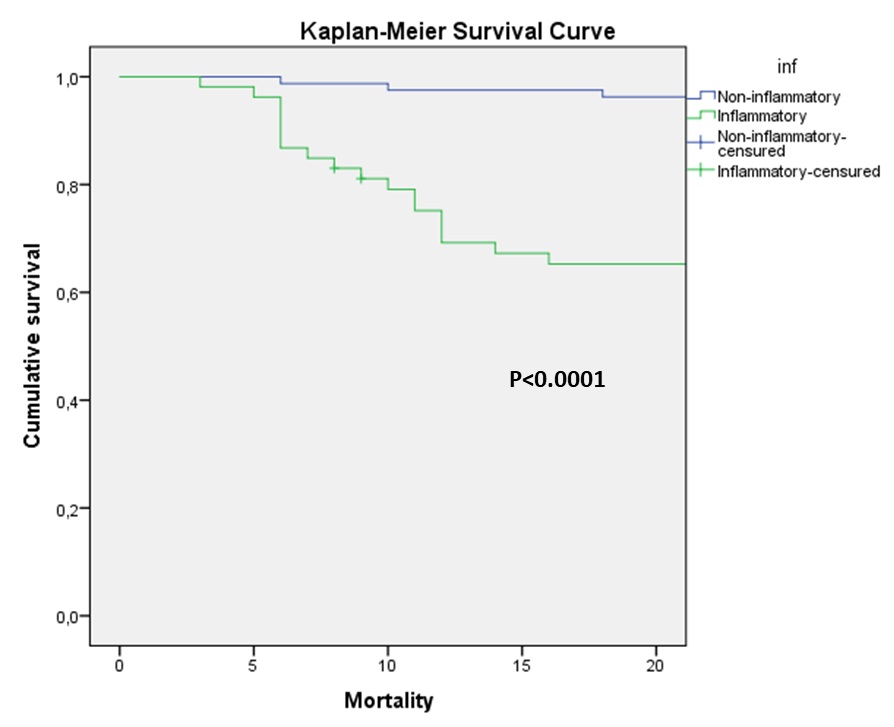
Results: Among 133 patients, 53 (39%) exhibited a persistent inflammatory phenotype. Inflammatory phenotype was more frequently associated with diffuse-cutaneous disease (p=0.02), anti-Scl-70 autoantibodies (p=0.02), ILD (p=0.02), lower diffusing capacity for carbon monoxide (p=0.01) and myositis (p=0.04) (Table 1). Higher serum levels of KL-6 (p=0.002) and IL-18 (p=0.04) at baseline were observed in patients with an inflammatory phenotype. Those with persistent inflammation had a 4.6 times higher risk of all-cause mortality (HR 4.61 [95% CI 1.2-15.2, p=0.04) and 5.6 times higher of ILD (HR 5.41 [95%CI 2.4-16.4], p=0.02) compared to non-inflammatory patients (figure 1 and figure 2). Logistic regression linked inflammation with mortality (β=0.65, p=0.004), ILD (β=0.45, p=0.007), arthritis (β=0.40, p=0.04), myositis (β=0.23, p=0.04), IL-18 levels (β=0.32, p=0.002) and anti-Scl70
positivity (β =0.21, p=0.04).
Conclusion: The study linked persistent inflammation in SSc patients to distinct clinical and immunological features. Importantly, patients with persistent inflammation had substantially increased risks of all- cause mortality and ILD. These findings highlight the prognostic value of recognizing and monitoring the inflammatory phenotype in SSc patients for more targeted management approaches.
To cite this abstract in AMA style:
sieiro santos c, Retuerto M, Pérez García P, Ordas Martínez J, Baenas P, Moriano Morales C, Díez Álvarez E. The Role of Inflammation in Systemic Sclerosis: CRP-Associated Phenotypes and Prognostic Implications [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/the-role-of-inflammation-in-systemic-sclerosis-crp-associated-phenotypes-and-prognostic-implications/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-role-of-inflammation-in-systemic-sclerosis-crp-associated-phenotypes-and-prognostic-implications/