Session Information
Date: Monday, November 13, 2023
Title: (1365–1382) Sjögren’s Syndrome – Basic & Clinical Science Poster I
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: To investigate the prevalence of anti-thyroid autoantibodies, abnormal thyroid function, and their clinical impacts in Korean patients with primary Sjögren’s syndrome (pSS).
Methods: One hundred ninety-six pSS patients (190 females; median age 58.6 [IQR, 46.5-67.3]), satisfying the 2016 ACR/EULAR criteria, were consecutively enrolled. Those with a history of overt thyroid disease (n=22) or thyroid cancer (n=4) were excluded. Clinical variables including EULAR Sjögren’s Syndrome Disease Activity Index (ESSDAI) and Patient Reported Index (ESSPRI) were collected. For the relative contribution of fatigue to ESSPRI, the fraction of fatigue (Ffatigue) was calculated using ESSPRI fatigue score/ESSPRI score. Laboratory data including the complete blood count, ESR, and levels of thyroid-stimulating hormone (TSH; uIU/mL), free T4 (ng/dL), IgG, β2-microglobulin, cryoglobulin, and complement C3 and C4 were assessed. TSH/fT4 ratio was calculated. Anti-thyroglobulin (TG), anti-thyroperoxidase (TPO), TSH-binding inhibiting immunoglobulin (TBII), and anti-TSH receptor antibody (TSHR) were measured. Subclinical hypothyroidism (ST) was defined as TSH > 4.0 and the presence of hypothyroidism-related autoantibodies. The Mann-Whitney test, Chi-squared or Fischer’s exact test, and logistic regression analysis were performed.
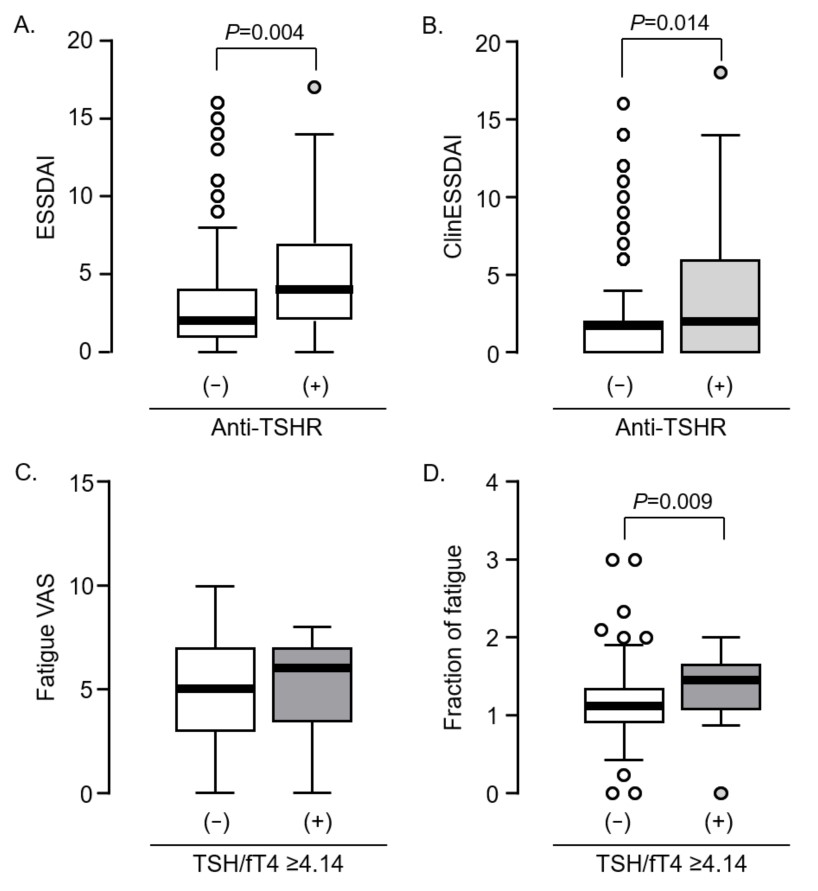
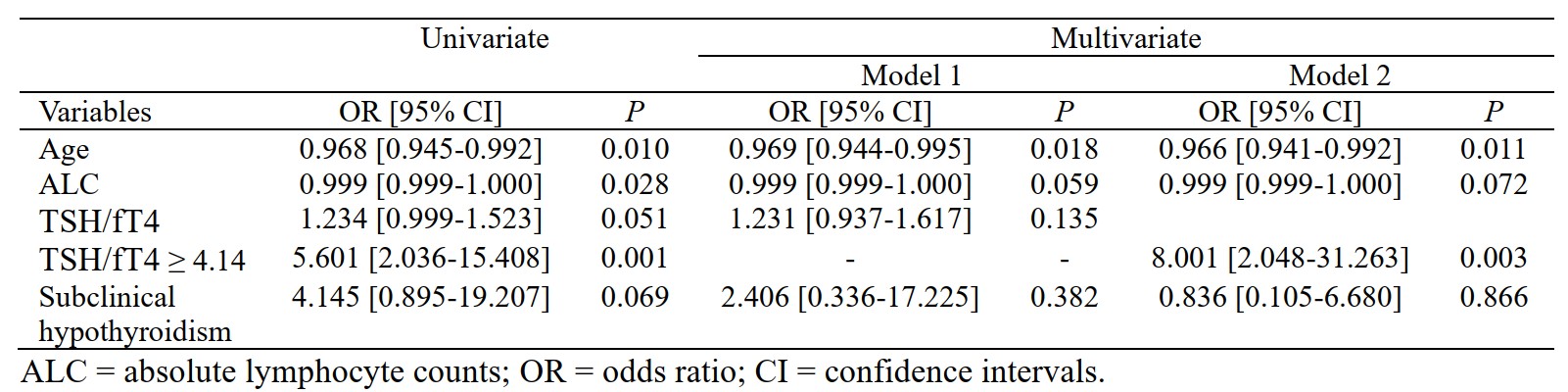
Results: Of 196 patients, 71 (36.2%) had one of the anti-thyroid autoantibodies and 53 (27%) had one of the hypothyroidism-related autoantibodies. The prevalence of anti-TG, anti-TPO, TBII, and anti-TSHR was 31 (15.8%), 28 (14.3%), 8 (4.1%), and 28 (14.3%), respectively. Twenty-four (12.2%) had TSH > 4.0 and 3 (1.5%) had TSH < 0.3. No patients had TSH > 10.0. ST was observed in 7 (3.6%) and was significantly associated with anti-TPO (p < 0.001) and TBII (p < 0.05). Patients with anti-TSHR had significantly higher levels of ESSDAI or clinical ESSDAI (both p < 0.05) and those with TSH/fT4 ≥ 4.14 had significantly higher Ffatigue levels (p < 0.01; Fig. 1). In multivariate logistic regression analyses, subclinical hypothyroidism (OR=5.61 [95% CI 1.07-29.50]) or TFI ≥ 4.14 (OR=9.01 [2.35-34.56]) was associated with the top quantile of Ffatigue. Additionally, TSH/fT4 ≥ 4.14 was an independent predictor for the highest quantile of Ffatigue (OR=8.00 [2.05-31.26]; Table 1).
Conclusion: Despite a high positive rate of thyroid-related autoantibodies, subclinical hypothyroidism was uncommonly observed in Korean pSS patients. The high TSH/fT4 ratio was significantly associated with “fatigue-dominance” in ESSPRI, and it may be related to the neuroendocrine aspects of fatigue in pSS.
To cite this abstract in AMA style:
Lee J, Choi S, Ha Y, Kang E, Kim K, Hyon J, Lee Y. The Relative Burden of Fatigue Is Associated with High TSH/fT4 Ratio in Korean Patients with Primary Sjogren’s Syndrome [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/the-relative-burden-of-fatigue-is-associated-with-high-tsh-ft4-ratio-in-korean-patients-with-primary-sjogrens-syndrome/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-relative-burden-of-fatigue-is-associated-with-high-tsh-ft4-ratio-in-korean-patients-with-primary-sjogrens-syndrome/