Session Information
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: For patients with autoimmune interstitial lung disease (ILD), the clinician’s interpretation of the extent of ground glass relative to fibrosis on imaging often influences the choice of treatment (immunomodulatory vs. antifibrotic therapy). However, it is unknown if the ground glass to fibrosis ratio affects treatment response for patients with different types of autoimmune ILDs. The purpose of this study is to examine the relationship between quantitative ground glass opacity to fibrosis ratio on baseline imaging and treatment response to immunomodulatory therapy in patients with ILD associated with systemic sclerosis (SSc) and rheumatoid arthritis (RA).
Methods: Participants of three independent cohorts were included in the present study: (1) Scleroderma Lung Study (SLS) I, which compared cyclophosphamide with placebo for SSc-ILD; SLS II, which compared cyclophosphamide with mycophenolate for SSc-ILD; and a retrospective cohort of patients with rheumatoid arthritis RA-ILD treated with immunomodulatory therapy (azathioprine, mycophenolate mofetil or rituximab). Pretreatment high-resolution computed tomography (HRCT) scans underwent quantitative image analysis to determine whole lung ground glass and fibrosis extent. Forced vital capacity (FVC) and diffusion capacity for carbon monoxide (DLCO) percent predicted were measured at baseline and 12-months. Logistic regression analysis was used to examine the relationship between baseline ground glass to fibrosis ratio and the following outcomes: FVC improvement of 3% or greater, FVC decline of 3% or greater, and FVC decline of 5% or more or DLCO decline of 10% or more. Two sample t-tests were performed to compare the mean change from baseline in FVC%-predicted between patients with high versus low fibrosis scores based on the median.
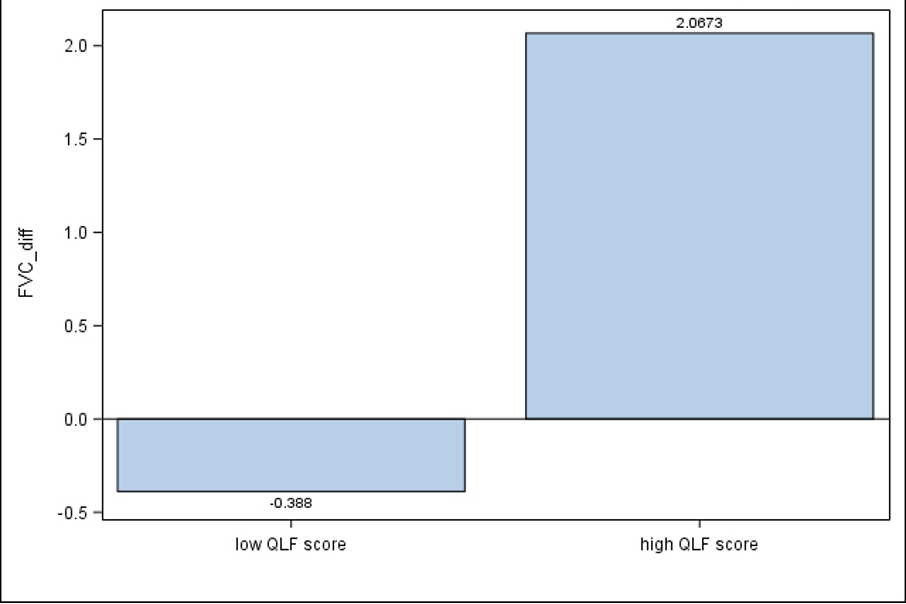
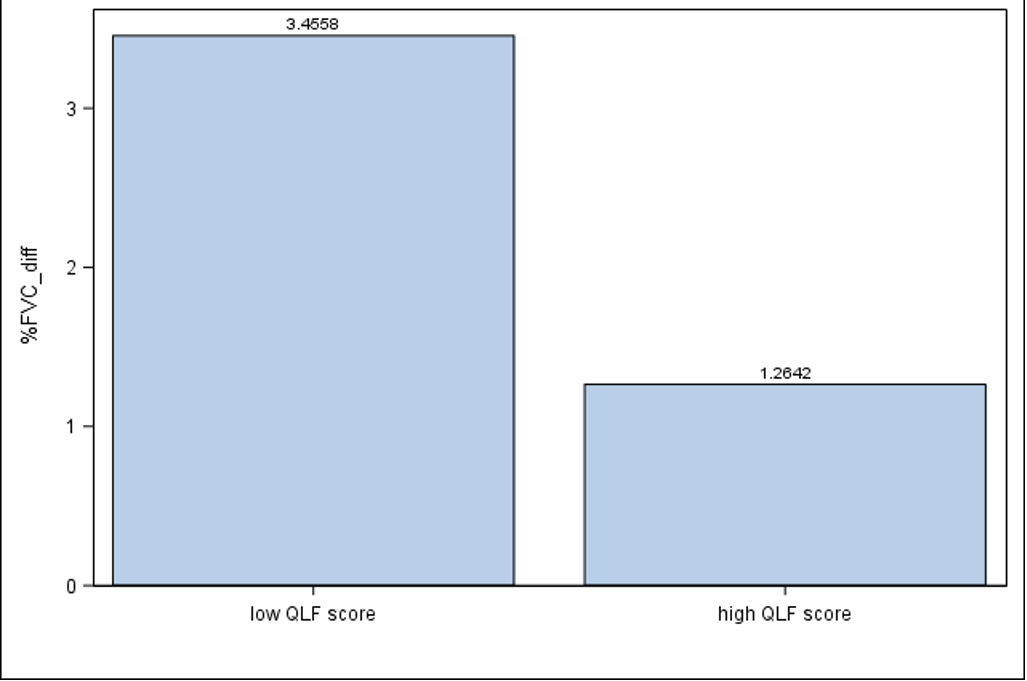
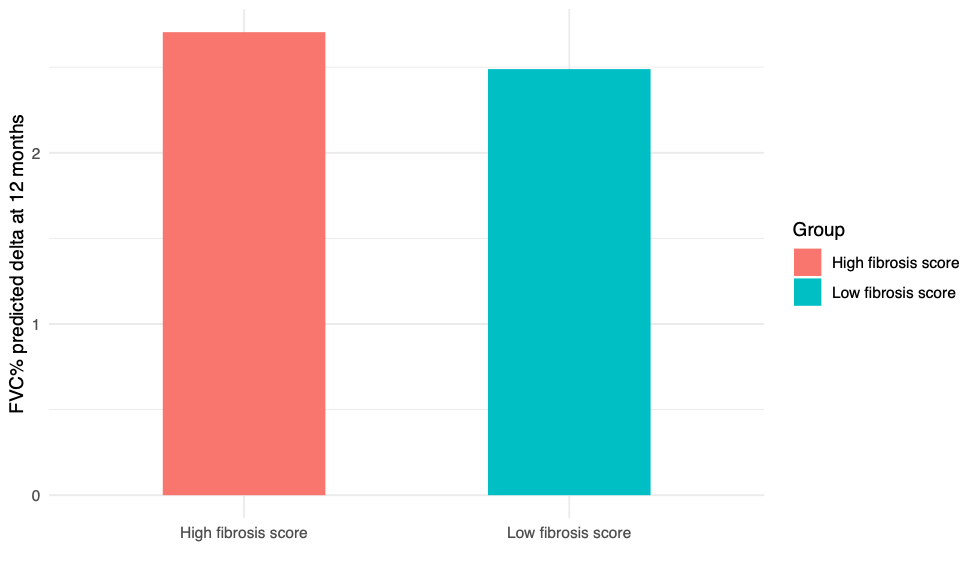
Results: The total cohort included 354 patients with autoimmune ILD. The mean baseline quantitative ground glass to fibrosis ratio at baseline was higher in the SSc cohorts (SLS I: 5.3 [SD 5.5], SLS II: 5.0 [SD 5.2]) than in the RA-ILD cohort (0.62 [SD 1.2]). No significant association was observed between the quantitative ground glass to fibrosis ratio and FVC improvement ≥3% or decline ≥3%, nor the physiologic criteria for progressive pulmonary fibrosis (FVC decline of 5% or more or DLCO decline of 10% or more) at one year in any of the cohorts. Participants with high fibrosis scores demonstrated improved response to treatment with CYC in SLS I and II (Figure 1), while participants with high versus low fibrosis scores experienced a similar improvement in FVC%-predicted in the SLS II-MMF arm (Figure 2) and the RA-ILD cohort (Figure 3).
Conclusion: The extent of ground glass relative to fibrosis does not appear to affect treatment response to immunomodulatory therapy in patients with SSc-ILD and RA-ILD; whereas, higher fibrosis extent was associated with improved response to CYC in SSc-ILD. While the presence of ground glass opacity may signify an underlying inflammatory process, the etiologies of this radiological phenomenon are diverse in these two diseases and additional research is needed to understand how to predict treatment response using radiological parameters in patients with autoimmune ILD.
To cite this abstract in AMA style:
Matson S, Humphries S, Lee j, Roth M, Tashkin D, Kim G, Goldin J, Leng M, Volkmann E. The Relationship Between the Extent of Ground Glass to Fibrosis Ratio and Treatment Response to Immunomodulatory Therapy in Three Separate Autoimmune Interstitial Lung Disease Cohorts [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/the-relationship-between-the-extent-of-ground-glass-to-fibrosis-ratio-and-treatment-response-to-immunomodulatory-therapy-in-three-separate-autoimmune-interstitial-lung-disease-cohorts/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-relationship-between-the-extent-of-ground-glass-to-fibrosis-ratio-and-treatment-response-to-immunomodulatory-therapy-in-three-separate-autoimmune-interstitial-lung-disease-cohorts/