Session Information
Session Type: Poster Session (Sunday)
Session Time: 9:00AM-11:00AM
Background/Purpose: The gastrointestinal (GI) tract is the most commonly affected internal organ system in systemic sclerosis (SSc), resulting in significant morbidity and mortality. Several studies that objectively evaluated GI tract dysfunction and abnormal transit in SSc have shown that such abnormalities associate inconsistently with clinical symptoms and severity, resulting in challenges related to diagnosis, risk stratification, and therapeutic interventions. We sought to determine whether clinical symptoms associate with objective evidence of GI dysmotility in SSc, and to determine how patterns of abnormal transit fit with existing GI symptom and severity scales in the field of scleroderma.
Methods: Patients with SSc and GI symptoms were recruited from clinic in the Johns Hopkins Scleroderma Center. Patients completed the UCLA GIT 2.0 survey, were assessed by the Medsger GI severity score, and underwent a nuclear medicine-based whole gut transit (WGT) study. The association between patient GI symptoms, GI severity, and characteristics of abnormal transit in each region of the GI tract were compared, and the association between areas of abnormal transit and GI severity was also examined.
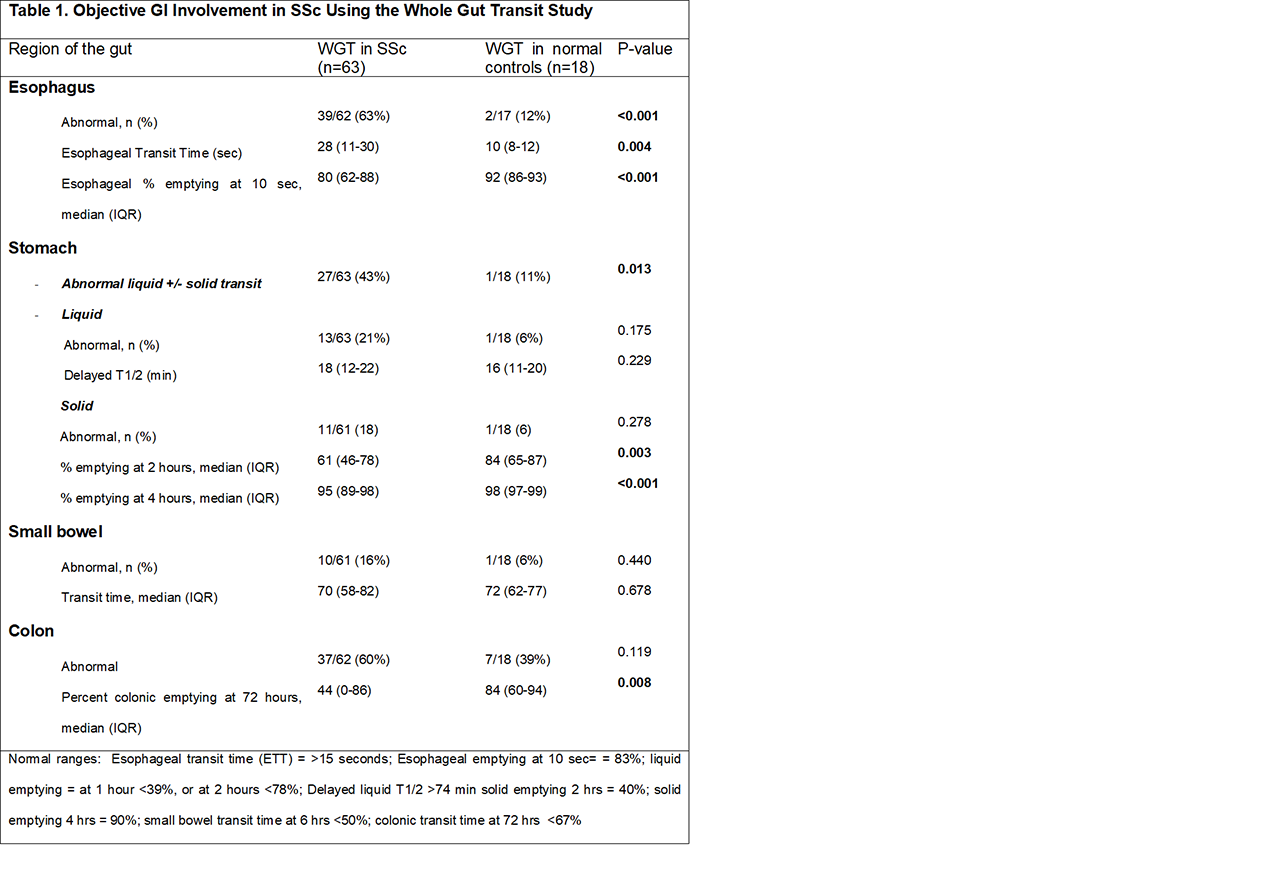
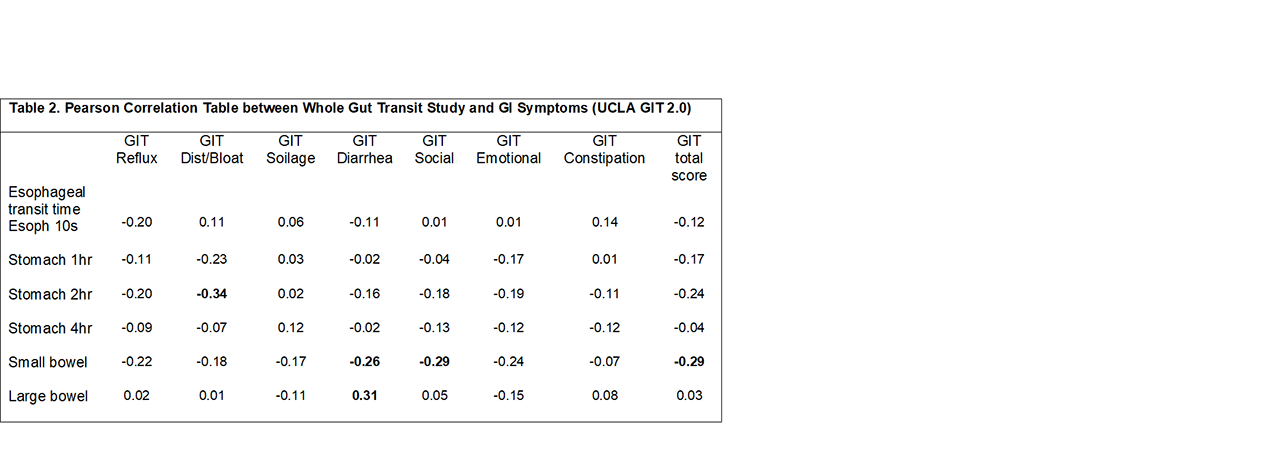
Results: WGT scintigraphy was performed on 63 SSc patients with active GI symptoms and 18 healthy controls. In the cohort, the average age was 58.4 years, with 84.1% being female and 80.6% being Caucasian. Median disease duration was 10 years, and 27.1% had diffuse cutaneous disease. Approximately 60% of SSc patients had more than one abnormal region on WGT studies. SSc patients were more likely to have delayed esophageal transit time [28% vs. 10%; p=0.004], delayed esophageal percentage emptying at 10 seconds [80% vs 92%; p=< 0.001], delayed gastric emptying at both 2 hours [61% vs. 84%; p=0.003] and 4 hours [95% vs. 98%; p< 0.001], and delayed colonic emptying at 72 hours [44% vs. 84%; p=0.008] compared to healthy controls (Table 1). Evaluating the association between Medsger GI severity scores (MGISS) and WGT results, patients with MGISS of 2 had slower esophageal transit and more gastroparesis compared to other Medsger groups. Patients with pseudo-obstruction and/or malabsorption (MGISS=3) were significantly more likely to have severe colonic delay (p< 0.05). Patients requiring total parenteral nutrition (MGISS=4) were significantly more likely to have small bowel dysmotility (p< 0.05). When comparing symptoms assessed by the UCLA GIT 2.0 with WGT measurements, symptoms of distention and bloating were inversely associated with percent gastric emptying at 2 hours (r=-0.34; p=0.011), and symptoms of diarrhea were positively associated with higher colonic transit times (r=0.031; p=0.026) (Table 2).
Conclusion: WGT provides a non-invasive assessment of bowel dysfunction and defines specific anatomical areas that associate with clinical symptoms and GI severity. This has implications not only in enhancing our understanding of symptom etiology, but also to guide therapy. These results are exciting in the face of known challenges in capturing objective pathology in SSc GI disease, and determining the association with active GI symptoms and outcome measures.
To cite this abstract in AMA style:
McMahan* Z, Tucker* A, Perin J, Pasricha J, Ziessman H, Rosen A, Wigley F. The Relationship Between Gastrointestinal Symptoms and Severity and Whole Gut Transit in Patients with Systemic Sclerosis [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/the-relationship-between-gastrointestinal-symptoms-and-severity-and-whole-gut-transit-in-patients-with-systemic-sclerosis/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-relationship-between-gastrointestinal-symptoms-and-severity-and-whole-gut-transit-in-patients-with-systemic-sclerosis/