Session Information
Date: Sunday, November 17, 2024
Title: SpA Including PsA – Diagnosis, Manifestations, & Outcomes Poster II
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Axial spondyloarthritis (axSpA) is a group of disorders typically occurring before the age of 45 whose common features include disabling inflammatory arthritis of the spine. AxSpA has been diagnosed using radiographs as part of modified New York criteria; however, radiographic damage may not appear in early disease, whereas magnetic resonance imaging (MRI) can detect sacral inflammation thereby identifying early disease patients. Despite this, the incidence of abnormal sacral MRIs is unknown in a young, community-based population with chronic inflammatory back pain (IBP) seeking primary care. Although point prevalence of axSpA in the U.S. has been about 1%, the number of patients with early undiagnosed disease is unknown. The incidence of MRI abnormalities accompanying the diagnosis of axSpA has been studied in specialty (orthopedic, rheumatologic) clinics, but the incidence of MRI positive sacroiliitis has not been adequately assessed in the primary care setting. For this reason, the study reported herein aims to determine the incidence of abnormal MRIs consistent with sacroiliitis among patients in the primary care setting who report at least 3 of 5 IBP features lasting 3 months or longer. The secondary objective is to determine, among patients with abnormal and normal MRIs, the proportions of those who are HLA-B27 positive.
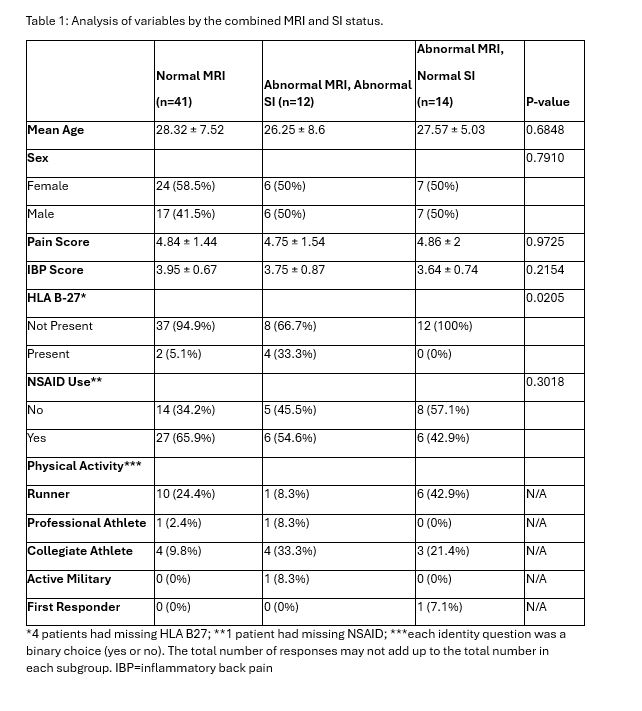
Methods: This is a prospective study of consecutively encountered adult patients younger than 45 years of age who presented to primary care chiropractic clinics with chronic low back pain and were then screened using an IBP assessment. If patient responses were positive for ≥3 out of 5 questions, MRI and HLA-B27 testing were obtained. Analysis of variance methods were used to determine the difference of outcomes among the groups. Crosstab Chi-square tests were conducted to assess the association between categorical outcomes and groups.
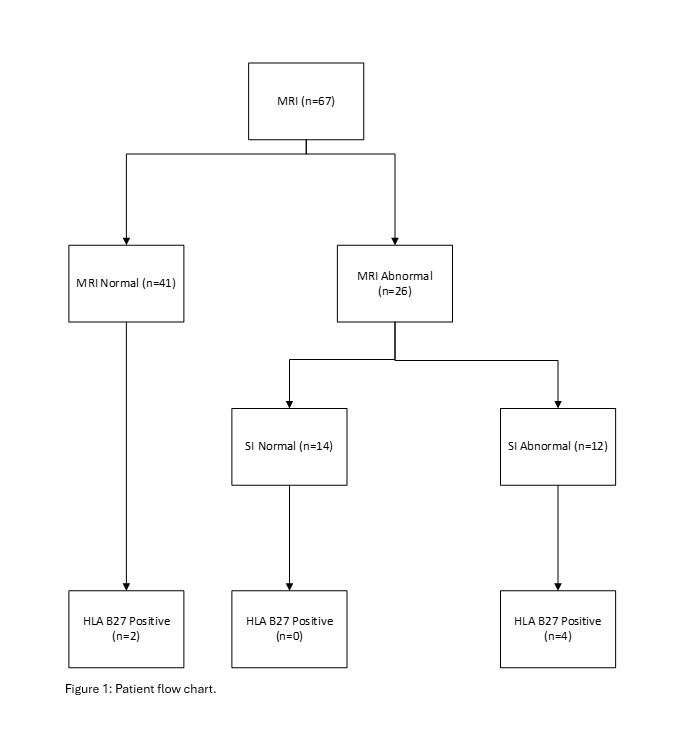
Results: We examined 67 MRIs using both T1 and Short Tau Inversion Recovery protocols from enrolled subjects screened positive for IBP. Of the 67 subjects, 41 had normal MRIs and 26 were abnormal. Among those 26 patients with abnormal MRIs, 12 (46.2%) were related to the SI joints, and the other 14 abnormal MRI patients did not have SI joint related abnormalities. Seven (26.7%) of the 26 subjects had hip abnormalities, two (7.7%) of which had synovitis/effusions in both hips and SI joints. There was a statistically significant association between the HLA B-27 and MRI sacroiliac (SI) joint status (p=0.0205). Specifically, 4 (33.3%) of the 12 with SI joint MRI abnormalities had a positive HLA B-27, none of the 14 normal SI but abnormal MRI patients had positive HLA B-27. For comparison, only 2 (4%) of the 41 normal MRI patients had positive HLA B-27.
Conclusion: Almost 40% (26 of 67) of patients with IBP symptoms had an abnormal sacral MRI. Of those 26, 46.2% (12 of 26) had abnormal SI joints. There was a statistically significant association between HLA B-27 and MRI SI joint abnormalities. We also found a substantial number of abnormal hip findings in this young population. Future research with a larger sample size is warranted to confirm the current findings.
To cite this abstract in AMA style:
Katsaros E, Russel R, Nagare M, Ochoa C, Dong F, Weisman M. The Proportion of Inflammatory Back Pain Patients with an Abnormal Sacral MRI in a Community-Based Primary Care Setting [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/the-proportion-of-inflammatory-back-pain-patients-with-an-abnormal-sacral-mri-in-a-community-based-primary-care-setting/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-proportion-of-inflammatory-back-pain-patients-with-an-abnormal-sacral-mri-in-a-community-based-primary-care-setting/