Session Information
Date: Sunday, October 26, 2025
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Patients with psoriatic arthritis (PsA) are at increased risk of developing cardiovascular diseases, including arrhythmias. Given that traditional cardiovascular disease risk factors are prevalent in patients with PsA, it remains unclear if arrhythmia development risk in this population is due to these factors or PsA disease activity. We therefore aimed to assess the incidence and risk factors for tachy- and bradyarrhythmias in patients with PsA.
Methods: We performed a retrospective cohort analysis of PsA patients followed prospectively from 1994 to 2024. Patients were assessed every 6 to 12 months following a standard protocol where demographics, measures of PsA disease activity, comorbidities and medication information were collected. Arrhythmia events were identified via review of patients charts and linkage with provincial hospitalization databases. The following arrhythmia endpoints were assessed: atrial tachyarrhythmia (defined as atrial fibrillation, atrial flutter or supraventricular tachycardia); bradyarrhythmia/pacemaker (defined as second degree atrioventricular block, complete heart block or pacemaker placement); ventricular tachyarrhythmia (defined as ventricular tachycardia, ventricular fibrillation or placement of implantable cardioverter-defibrillator). The cumulative incidence rate (CIR) of each type of arrhythmia was calculated. Cox regression hazard models were used to evaluate the association between PsA disease activity measures (either single time-point level prior to event or cumulative average over time) and arrhythmia endpoints. Each model was hierarchically adjusted for age and sex, PsA duration, cardiovascular risk factors and PsA therapies.
Results: Of 1670 PsA patients (mean age 46.3 years, 54.2% male, Table 1) included in this analysis, a total of 80 atrial, 17 brady and 11 ventricular arrhythmias were identified. By age 70, the overall CIRs were 7.82%, 0.45% and 0.67% for atrial, brady and ventricular arrhythmias, respectively (Figure 1). Arrhythmias occurred predominantly in older patients, with a marked increase in the rate of atrial tachyarrhythmias after age 60. Bradyarrhythmia and ventricular tachyarrhythmia also occurred predominantly in older population, with a marked increase in the rate of these events after age of 70. In the fully adjusted multivariable analysis (Table 2), remission/low vs. high disease activity state was associated with lower risk of atrial tachyarrhythmia (single-point Hazard Ratio (HR) 0.49, 95% CI 0.26, 0.92; cumulative mean HR 0.46, 95% CI 0.23, 0.91). Similarly higher 3-item Visual Analog Scale (3-VAS) was associated with higher risk of atrial tachyarrhythmia (single-point HR 1.18, 95% CI 1.04, 1.33; cumulative mean HR 1.22, 95% CI 1.04, 1.44). Although higher PASI scores showed a trend towards increased risk of arrhythmia, these findings did not reach statistical significance.
Conclusion: Higher PsA disease activity is associated with higher atrial tachyarrhythmia risk. These findings reinforce the importance of controlling inflammation in PsA to prevent these events.
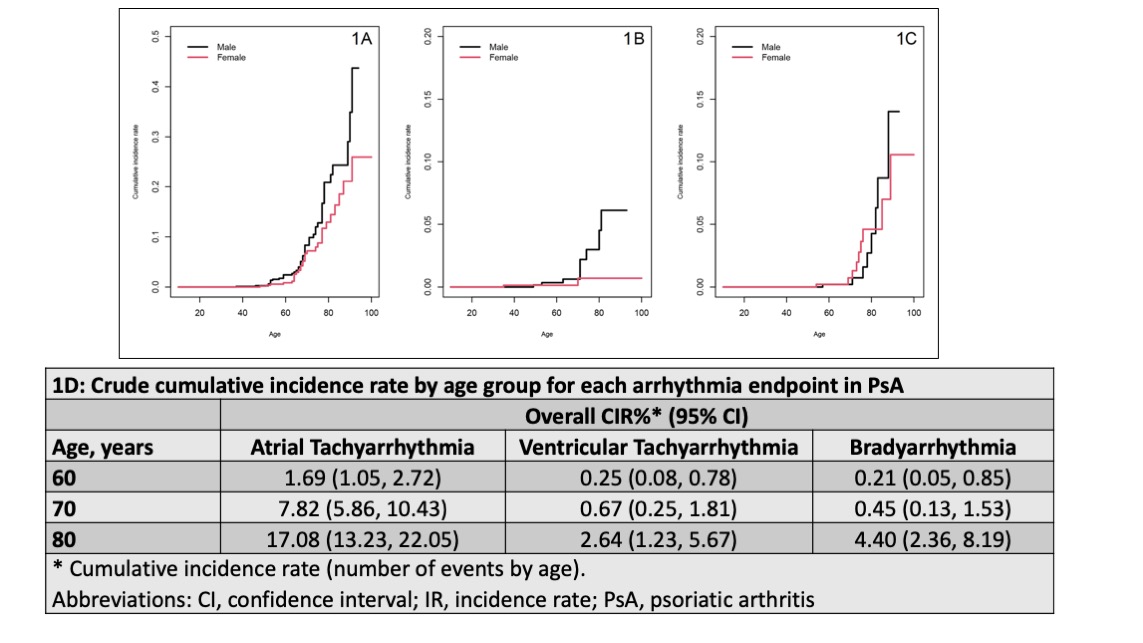 Table 1 : Baseline characteristics of the study population overall and among patients with arrhythmia
Table 1 : Baseline characteristics of the study population overall and among patients with arrhythmia
.jpg) Figure 1 – Cumulative incidence of arrhythmia events in male and female patients with PsA: 1A. Atrial Tachyarrhythmia; 1B. Ventricular Tachyarrhythmia; 1C. Bradyarrhythmia; 1D: Overall cumulative incidence rate by age (95% CI).
Figure 1 – Cumulative incidence of arrhythmia events in male and female patients with PsA: 1A. Atrial Tachyarrhythmia; 1B. Ventricular Tachyarrhythmia; 1C. Bradyarrhythmia; 1D: Overall cumulative incidence rate by age (95% CI).
.jpg) Table 2 – The association between PsA-related variables and the risk of atrial tachyarrhythmia in patients with PsA using Cox proportional hazards models
Table 2 – The association between PsA-related variables and the risk of atrial tachyarrhythmia in patients with PsA using Cox proportional hazards models
To cite this abstract in AMA style:
Almansouri A, Li J, Alhadri A, Colaco K, Harvey P, Ahktari S, Chandran V, Gladman D, Cook R, Eder L. The Incidence Rate and Risk Factors of Arrhythmias in Patients with Psoriatic Arthritis [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/the-incidence-rate-and-risk-factors-of-arrhythmias-in-patients-with-psoriatic-arthritis/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-incidence-rate-and-risk-factors-of-arrhythmias-in-patients-with-psoriatic-arthritis/
