Session Information
Date: Sunday, November 8, 2020
Title: SLE – Diagnosis, Manifestations, & Outcomes III: Lupus Nephritis (1512–1516)
Session Type: Abstract Session
Session Time: 4:00PM-4:50PM
Background/Purpose:
A major complication of systemic lupus erythematosus (SLE) is the progression of lupus nephritis (LN) to end-stage kidney disease (ESKD). Both SLE and ESKD are associated with increased risks of cardiovascular disease (CVD). Renal transplantation improves survival among patients with LN-ESKD. We sought to assess the potential impact of renal transplantation on CVD events in LN-ESKD.
Methods:
We identified all incident cases of ESKD due to SLE (ICD9 710.0) in the United States Renal Data System (USRDS) between 2000 and 2014. The USRDS captures nearly all patients with ESKD in the US and includes the cause of ESKD by ICD9 code as well as demographics, comorbidities, and dates of waitlist entry, transplantation and death including the cause of death. Hospitalizations are additionally captured under Medicare Part A. We restricted our study population to patients who were waitlisted for transplant to limit the potential bias of confounding by indication and required Medicare enrollment. To account for time-varying variables, we performed sequential cohort matching on the basis of age, sex, and time since initiation of dialysis.We sequentially matched patients on their transplant date (index date) 1:1 with comparators who remained active on the waitlist on that date. Follow-up began at the date of transplant or matching and ended at the time of death, end of Medicare coverage, three years following the index date, transplantation (control group only, at which point a participant would be matched and begin follow-up time in the transplant group), or January 1, 2015, whichever came first. The outcomes of interest were CVD events, including non-fatal and fatal myocardial infarctions (MI) and non-fatal and fatal cerebrovascular accidents (CVA). We determined CVD event rates in the groups that did and did not have transplants, accounting for competing risk of death, and calculated hazard ratios (HRs) using a stratified Cox proportional hazards model, additionally adjusting for race/ethnicity, time on waitlist, first ESKD treatment modality, ESKD-specific comorbidity score, Organ Procurement and Transplant Network region, and history of any organ transplant.
Results:
We identified 1,250 patients who had a transplant and 1,250 matched comparators. These groups were well-balanced by age, sex, time since initiation of dialysis, and time since entry onto the waitlist (Table 1). Over mean 2.26 years of follow up, 24 patients who had a transplant and 68 who did not have a transplant had a CVD event, yielding CVD event rates of 7.2 per 1000 person-years and 29.6 per 1000 person-years, respectively (HR, 0.56 [95% CI, 0.51-0.61]) (Table 2). After adjustment for covariates, the HR was 0.55 (95% CI, 0.50- 0.60). The findings were similar within subgroups by age, sex, and African American race. The adjusted HRs were 0.54 (95% CI, 0.50-0.59) for MI and 0.54 (95% CI, 0.50-0.59) for CVA.
Conclusion:
In this nationwide study of ESKD due to LN, renal transplantation was associated with a reduced risk of CVD events, including MI and CVA. Our findings highlight the importance of identifying barriers to transplantation in this population, as improved access could reduce CVD morbidity and mortality.
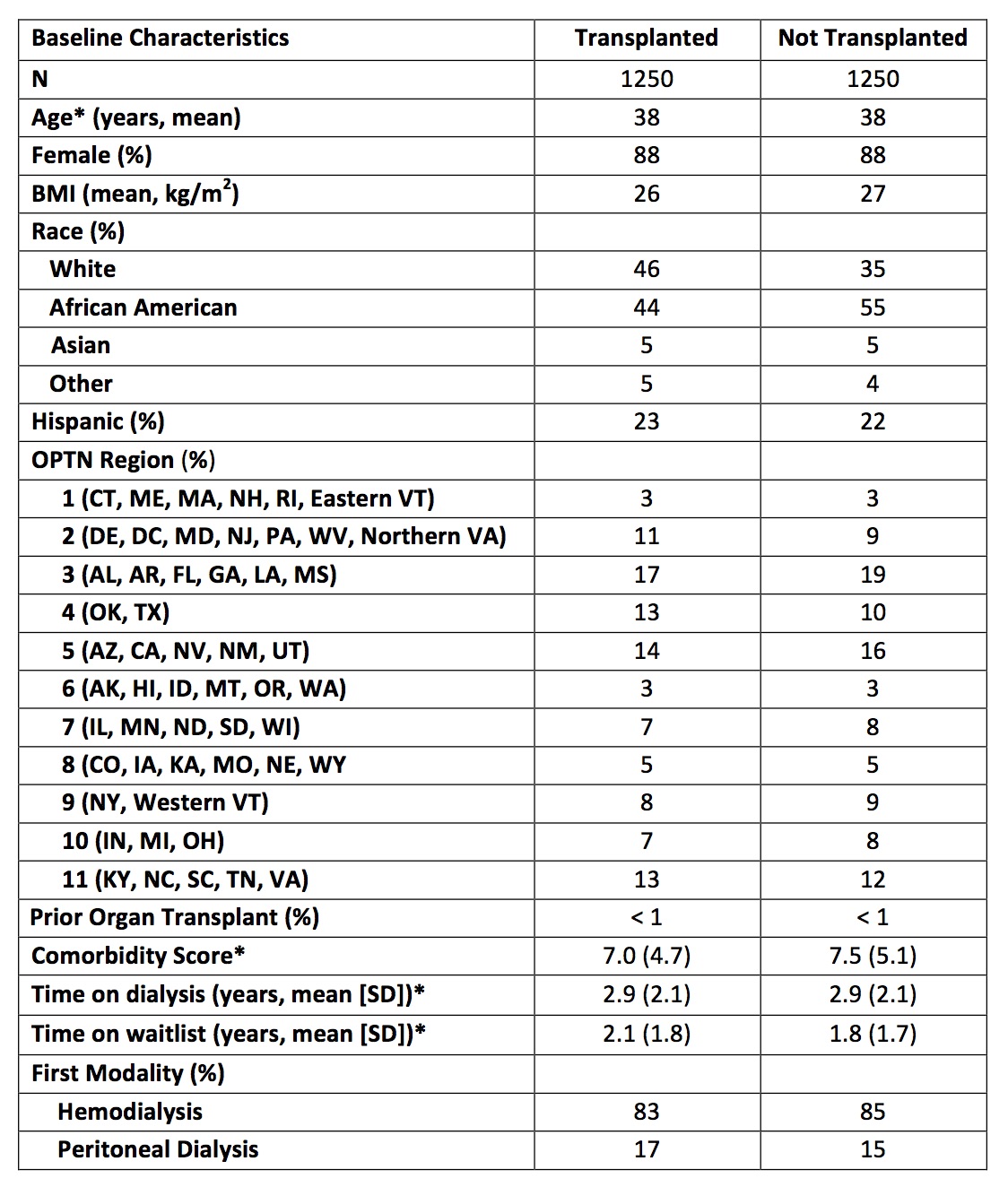 Table 1. Characteristics of Patients with End-Stage Kidney Disease Due to Lupus Nephritis, Transplanted and Matched Comparators
Table 1. Characteristics of Patients with End-Stage Kidney Disease Due to Lupus Nephritis, Transplanted and Matched Comparators
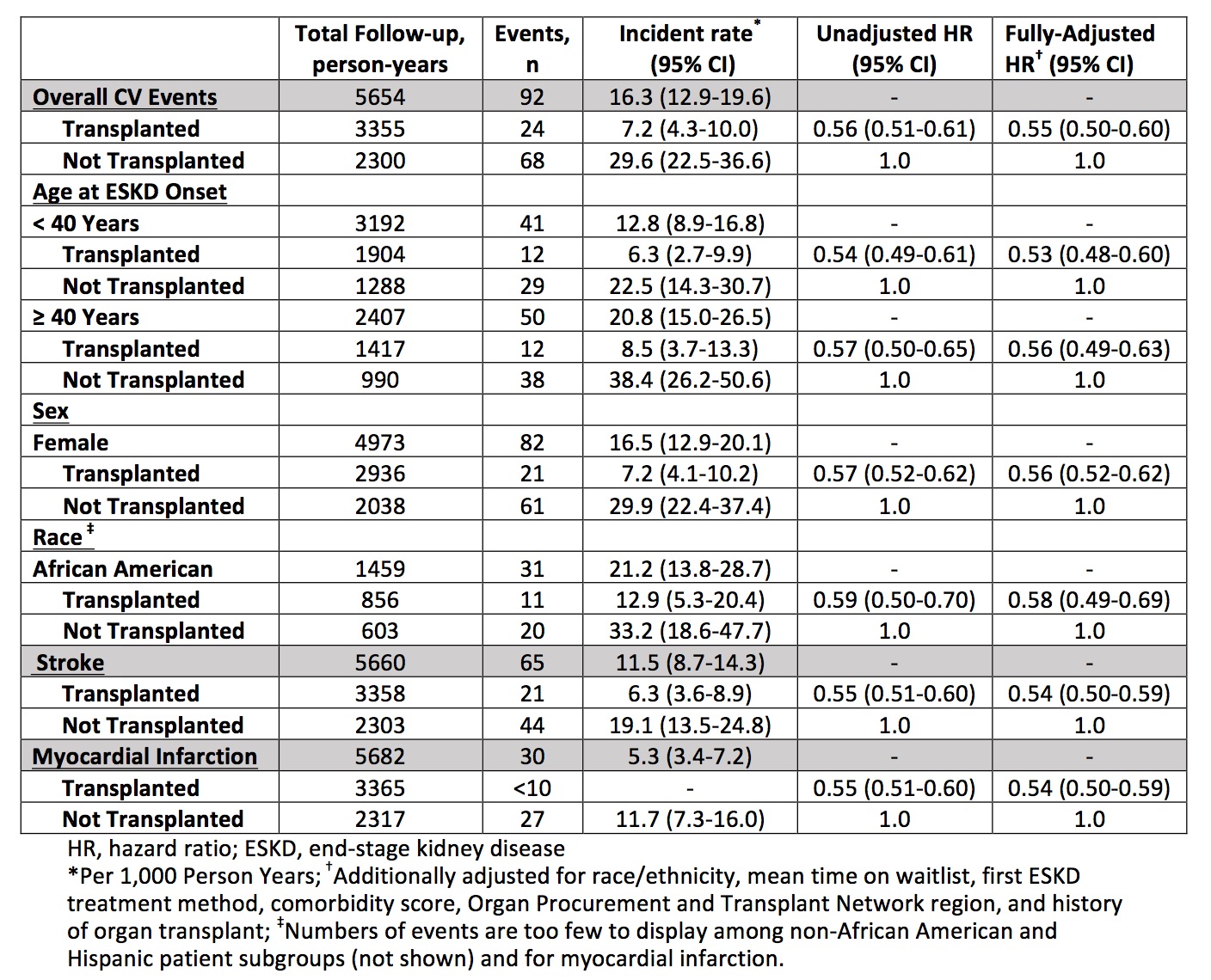 Table 2. Cardiovascular Events According to Transplant Status Among Matched Patients with End-Stage Kidney Disease Due to Lupus Nephritis
Table 2. Cardiovascular Events According to Transplant Status Among Matched Patients with End-Stage Kidney Disease Due to Lupus Nephritis
To cite this abstract in AMA style:
Jorge A, Fu X, Zhang Y, Choi H, Wallace Z. The Impact of Renal Transplantation on Cardiovascular Events Among Patients with End-State Kidney Disease Due to Lupus Nephritis: A Nationwide Cohort Study [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/the-impact-of-renal-transplantation-on-cardiovascular-events-among-patients-with-end-state-kidney-disease-due-to-lupus-nephritis-a-nationwide-cohort-study/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-impact-of-renal-transplantation-on-cardiovascular-events-among-patients-with-end-state-kidney-disease-due-to-lupus-nephritis-a-nationwide-cohort-study/
