Session Information
Date: Monday, October 27, 2025
Title: (1517–1552) Systemic Lupus Erythematosus – Treatment Poster II
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Type I interferon (IFN) signaling is central to systemic lupus erythematosus (SLE) pathogenesis, and anifrolumab, a monoclonal antibody targeting the IFN-α receptor (IFNAR), has emerged as a promising therapy. This systematic review evaluates the impact of baseline IFN signature on anifrolumab’s efficacy and safety and synthesizes its overall clinical profile in SLE.
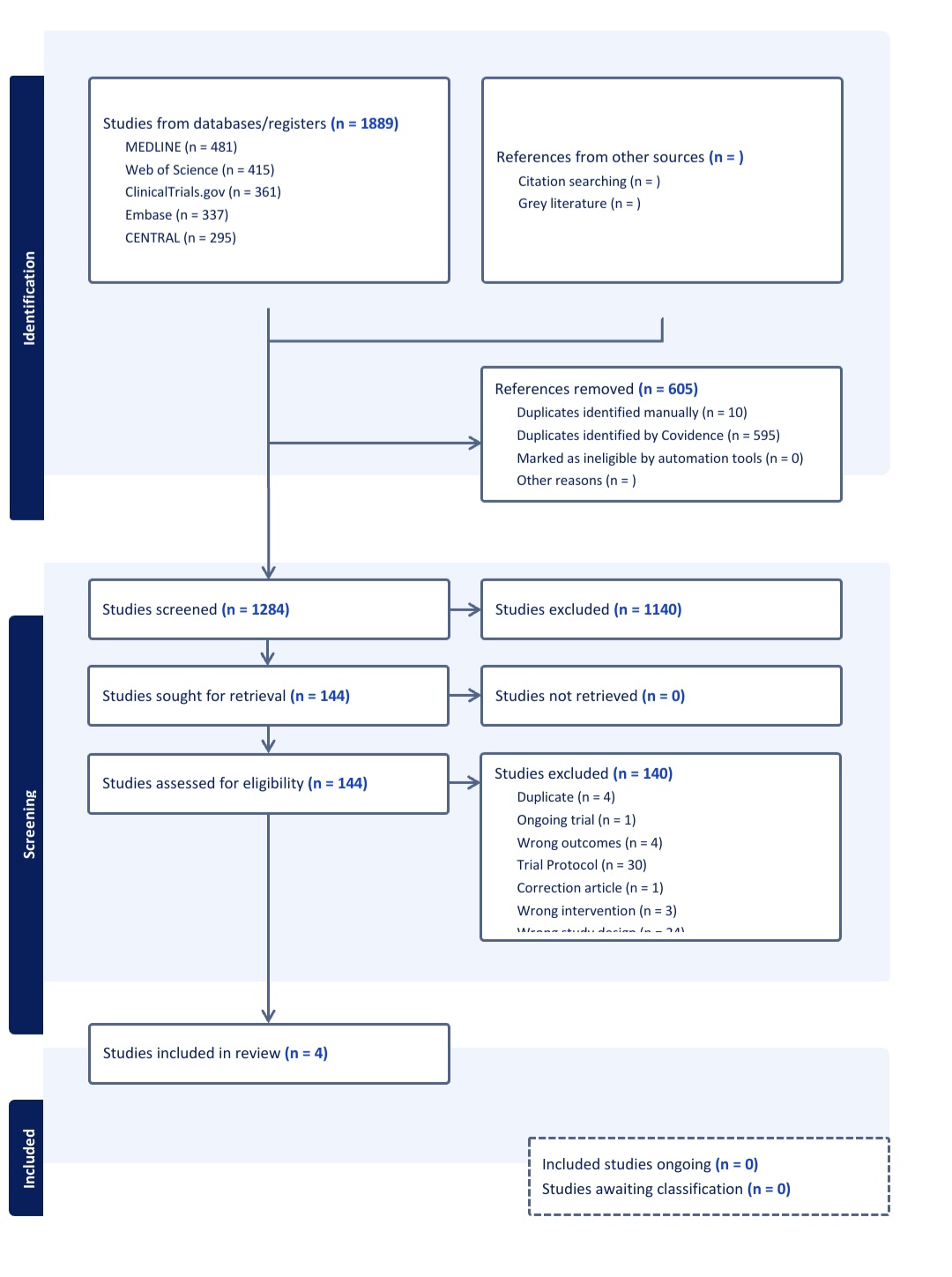
Methods: A comprehensive systematic review was conducted in accordance with PRISMA guidelines. We analyzed data from four randomized controlled trials (RCTs, n = 1,271 patients) comparing anifrolumab (150–1,000 mg) to placebo. Primary outcomes included SLE Responder Index-4 (SRI-4), BILAG-Based Composite Lupus Assessment (BICLA), and IFN signature-stratified efficacy/safety. Secondary outcomes assessed pooled efficacy and adverse events. Risk of bias was assessed using the Cochrane Risk of Bias 2.0 tool across five domains. Two reviewers independently evaluated the studies, and discrepancies were resolved by consensus.
Results: Patients with high baseline IFN signatures (measured via 4- or 21-gene assays) demonstrated superior clinical responses. In phase 3 trials, anifrolumab 300 mg achieved significantly higher BICLA response rates versus placebo (47.8% vs. 31.3%, *p* < 0.001), particularly in high IFN subgroups. SRI-4 responses were 36.1% (anifrolumab) vs. 40.2% (placebo) in TULIP-1 (*p* = 0.03), with enhanced efficacy in IFN-high patients. In lupus nephritis, an intensified anifrolumab regimen (900 mg induction) reduced urine protein-creatinine ratio (UPCR) in 84.3% vs. 73.5% placebo. However, IFN-high patients faced elevated infection risks (e.g., herpes zoster: 10/45 vs. 8/49 placebo). Pooled analysis revealed anifrolumab increased SRI-4 likelihood (RR = 1.4, 95% CI: 1.1–1.8) but raised serious infections (13.9% vs. 16.3% placebo). Upper respiratory infections (15–30%) and infusion reactions (10–15%) were common. Most included RCTs showed low risk of bias.
Conclusion: Anifrolumab is efficacious in SLE, with maximal benefit in IFN-high patients, though this subgroup requires vigilant monitoring for infections. These findings underscore the IFN signature’s role as a predictive biomarker and highlight the need for personalized risk-benefit assessment in SLE management.
 The forest plots showing efficacy of Anifroulomab
The forest plots showing efficacy of Anifroulomab
.jpg) PRISMA Flow Chart Showing The Details of Included Databases and Studies
PRISMA Flow Chart Showing The Details of Included Databases and Studies
.jpg) PLOTS FOR RISK OF BIAS ASSESSMENT
PLOTS FOR RISK OF BIAS ASSESSMENT
To cite this abstract in AMA style:
Hashmi M, Piranavan P, Sufi Y, Nasir Z, Azhar Z, Tariq S, Ul Hudaibia H, SAEED I, Zulfiqar A, Rasool N, Faiz A. The Impact Of Interferon Signature On Anifrolumab Efficacy And Safety In Systemic Lupus Erythematosus: A Systematic Review And Meta-analysis [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/the-impact-of-interferon-signature-on-anifrolumab-efficacy-and-safety-in-systemic-lupus-erythematosus-a-systematic-review-and-meta-analysis/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-impact-of-interferon-signature-on-anifrolumab-efficacy-and-safety-in-systemic-lupus-erythematosus-a-systematic-review-and-meta-analysis/
