Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Gout is characterized by chronic inflammatory arthritis caused by the deposition of monosodium urate crystals and leads to increased risk of complications, such as serious infections, and premature mortality. Variances in the onset and progression of gout have been studied, showing the influence of environmental-genetic interactions. However, the specific extent of regional variations in patients with gout and associated outcomes in the US still remains unclear.
Methods: We analyzed data from the 2018-2019 National Inpatient Sample (NIS) database to identify patients admitted with a principal diagnosis of gout and/or hyperuricemia. We compared categorical variables using chi-square tests and compared continuous variables with independent samples t-testing. To adjust for potential confounding variables, we employed logistic and linear regression models. Confounders were selected through a univariate screen with a p-value cutoff of less than 0.2. Also, the Charlson comorbidity index was used to account for comorbid conditions. Other hospital characteristics such as “academic status” or “bed size” were not included in the multivariate analysis as collinearity would lead to inaccurate results.
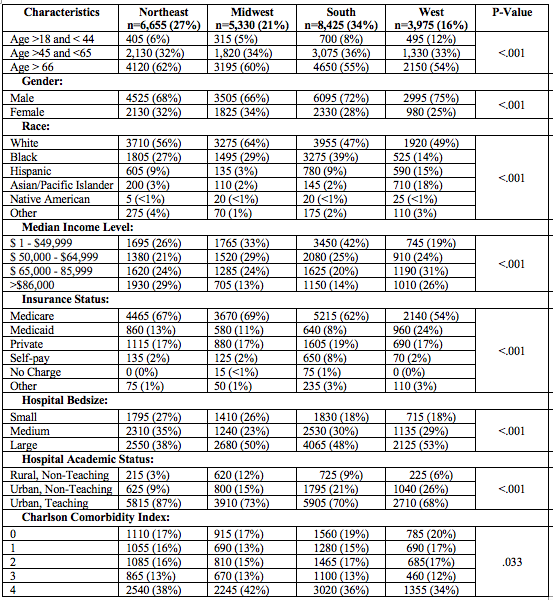
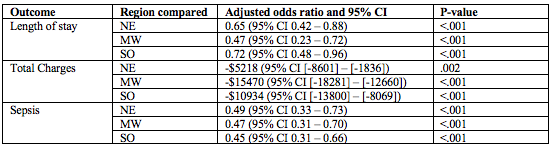
Results: In our analysis of the 2018-2019 NIS, we identified a total of 24,385 hospitalizations (weighted) with a principal diagnosis of gout of which 27% were admitted in northeastern (NE) regions, 21% at midwestern (MW) regions, 34% in southern (SO) regions, and 16% in western (WE) regions. In all the regions, majority of the admissions (greater than 55%) were patients over the age of 66 years, males and insured through Medicare. Interestingly, WE regions had the highest noted Asian/Pacific Islander admissions for gout with total of 710 patients (18%), in comparison to less than 3% in the other regions. Patients admitted in WE regions had a statistically significant increase in length of stay, as well as odds of sepsis when compared to the other regions (NE, MW, SO) [p-value =< .001]. In contrast, there was surprisingly a statistically significant decrease in total hospital charges in WE regions compared to all other regions [p-value=< .001]. There was no statistically significant difference in all-cause mortality.
Conclusion: This is a fundamental study using the NIS database to look at the differences in patients with gout and their outcomes in the various US regions. Our results showed a significant increase in sepsis and length of stay in WE regions. A theory could be the differences in social determinants of health influencing access to healthy diet, medication adherence and alcohol consumption. Furthermore, it is interesting to note that the WE regions had the highest proportion of Asian gout patients, who are known to have significantly increased prevalence and complications of gout. Thus, the race/ethnic variances, including the genetics, of our patients with gout should also be researched. In conclusion, our study highlights the need to move away from gout having a “One Plan Fits All” treatment, and further research needs to be done to look at differences in factors like race/ethnicity, genetics, cultural diets and seasonal/environmental changes to individualize treatment plans.
*Adjusted for age, gender, insurance status, and Charlson comorbidity index.
To cite this abstract in AMA style:
Rasheed N, ABDULLAH k, Reyes C. The Impact of Hospital Region on Mortality and Other Outcomes in Patients with Gout: A Two-Year Nationwide Analysis [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/the-impact-of-hospital-region-on-mortality-and-other-outcomes-in-patients-with-gout-a-two-year-nationwide-analysis/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-impact-of-hospital-region-on-mortality-and-other-outcomes-in-patients-with-gout-a-two-year-nationwide-analysis/