Session Information
Session Type: Poster Session C
Session Time: 1:00PM-3:00PM
Background/Purpose: Rheumatoid Arthritis (RA) is a systemic, inflammatory disease, and its burden extends beyond joint disease. RA is not commonly associated with central nervous system and brain changes. However, there is some evidence suggesting that there is a link between RA and cognitive impairment. There is limited information available in the literature regarding the prevalence, as well as the clinical and sociodemographic factors, that may contribute to cognitive dysfunction in RA. Reports of an association between disease activity in RA and cognitive dysfunction are inconsistent. This study aimed to evaluate the rate of patient-reported cognitive dysfunction and its association with disease activity using a very large, independent US registry.
Methods: We utilized data from the CorEvitas RA registry. A cross-sectional analysis used the latest patient visit available from 1/1/2011 to 12/31/2019 with information on the Clinical Disease Activity Index (CDAI), problems thinking, age and gender. The association of CDAI with patient- reported cognitive dysfunction (responded “yes” to the question asking if they had “problems with thinking”) was estimated using logistic regression models controlling for sociodemographic (age, gender, race, education, insurance), comorbidity (diabetes mellitus, fibromyalgia, body mass index, smoking, alcohol use), RA disease characteristics (disease duration, disability) and medication use (prednisone, NSAID, narcotic, biologic, tsDMARD and MTX). We further examined whether the relationship between disease activity and cognitive dysfunction varied based on patients age (< 55 vs ≥ 55 years) testing the moderating effect using a likelihood ratio test.
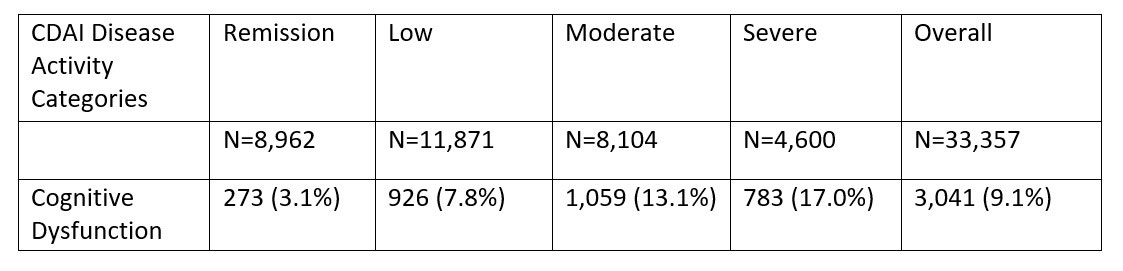
Results: A total of 3,041 of 33,537 patients (9.1%), reported cognitive dysfunction (Table 1). Those who reported cognitive dysfunction were more likely to be women (84.1% vs. 76.5%, p< 0.001), younger (60.7 vs. 62.5 years, p< 0.001), disabled (28.7% vs. 12.0%, p< 0.001), and have a higher mean CDAI 16.2 (SD: 12.5) vs 10.1 (SD: 10.8, p< 0.001). The adjusted odds ratio (OR) for low, moderate, and severe disease activity vs remission was 2.17 [95%CI: 1.88-2.50], 3.25 [95% CI: 2.82-3.75] and 3.83 [95%CI: 3.29-4.47] respectively (Table 2). Age had a moderating effect with the association of disease activity and self-reported cognitive dysfunction more pronounced in those aged < 55. The ORs for low, moderate, and severe disease activity were 3.29, 5.59, 5.76 respectively in age < 55 vs 1.90, 2.67, 3.37 respectively in age ≥ 55 (p=0.0001) (Figure 1).
Conclusion: Increasing disease activity is associated with a higher likelihood of reporting cognitive dysfunction. The effect was more pronounced in younger as opposed to older RA patients. The predominance of reported cognitive issues in younger patients was unexpected.
To cite this abstract in AMA style:
Pala O, Pappas D, Reed G, Kremer J. The Impact of Disease Activity on Patient-Reported Cognitive Dysfunction in Rheumatoid Arthritis [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/the-impact-of-disease-activity-on-patient-reported-cognitive-dysfunction-in-rheumatoid-arthritis/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-impact-of-disease-activity-on-patient-reported-cognitive-dysfunction-in-rheumatoid-arthritis/