Session Information
Date: Saturday, November 6, 2021
Title: Sjögren's Syndrome – Basic & Clinical Science Poster (0296–0322)
Session Type: Poster Session A
Session Time: 8:30AM-10:30AM
Background/Purpose: Diagnosis of primary Sjögren’s syndrome (pSS) is challenging due to the disease’s phenotypic heterogeneity. pSS patients frequently experience a prolonged period between symptomatic onset and diagnosis, hypothesised to prove detrimental to patient outcomes. The objective of this study was to describe the impact of delayed diagnosis on disease severity and patient outcomes in patients with pSS.
Methods: Data were drawn from the Adelphi Primary Sjögren’s Syndrome (pSS) Disease Specific Programme™, a real-world point-in-time survey of rheumatologists and their consulting pSS patients in the United States. Physicians provided data on patient demographics and clinical characteristics. Patients self-completed patient-reported outcome (PRO) tools; including the EuroQol 5-dimension 5-level utility score (EQ-5D), EuroQol visual analogue scale (EQ VAS), Work Productivity and Activity Impairment Index questionnaire (WPAI), and the Functional Assessment of Chronic Illness Therapy – Fatigue (FACIT-F). EULAR Sjögren’s Syndrome Disease Activity Index (ESSDAI) and EULAR Sjögren’s Syndrome Patient Reported Index (ESSPRI) proxy scores were calculated by assigning scores to physician-perceived severity in each of the associated domains. Patients were compared according to the time between onset of pSS symptoms and diagnosis (< 3 months, 3-6 months, 6-12 months, and >12 months). Analysis of variance and Kruskall-Wallis tests were used to examine the impact of delayed diagnosis on ESSDAI, ESSPRI and PRO measures, and Mann-Whitney U-test for physician-perceived current severity using < 3 months as the reference group.
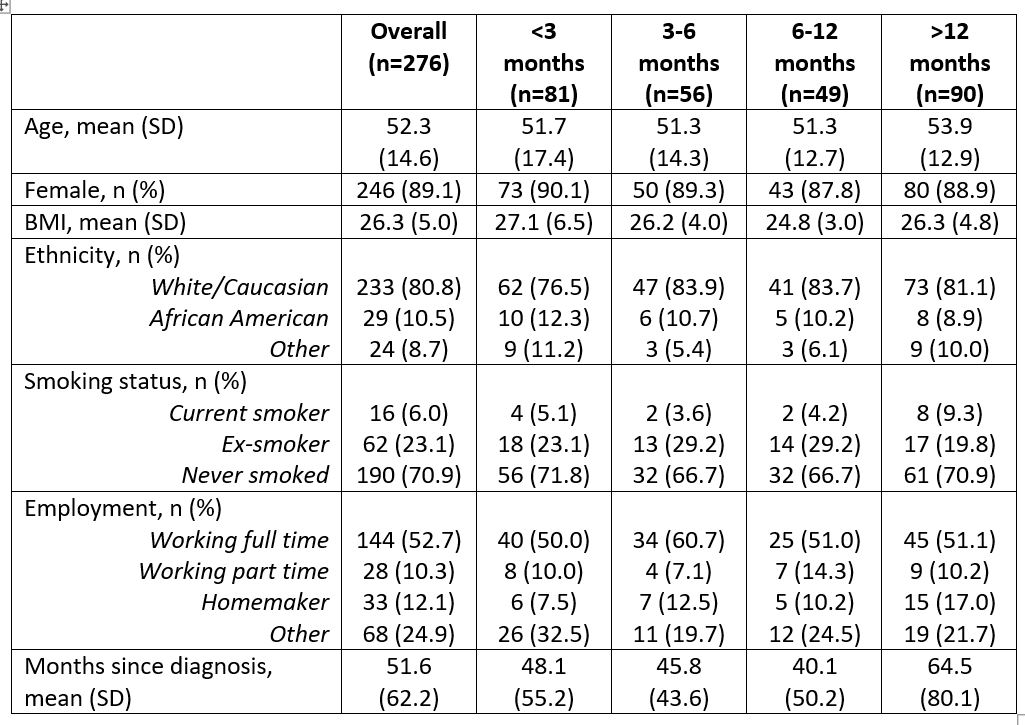
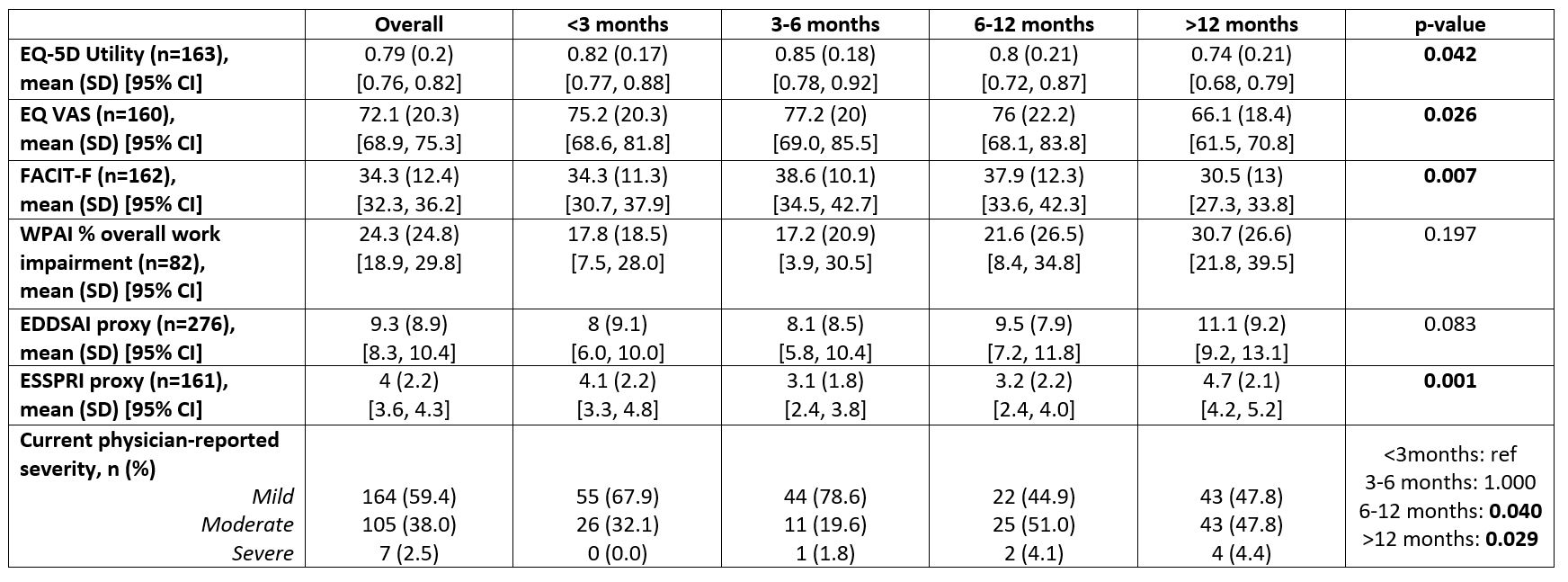
Results: 71 rheumatologists provided information for 276 pSS patients: mean age 52.3 years, 89.1% female and average time since diagnosis 51.6 months (Table 1). Of these patients, 29.3% were diagnosed within 3 months of the onset of pSS symptoms, 20.3% 3-6 months, 17.8% 6-12 months and 32.6% >12 months, with a mean (SD) of 27.5 (68.2) months from the onset of symptoms to diagnosis. Comparative analyses showed that there were significant differences (< 0.05) in EQ-5D utility score, EQ-5D VAS, FACIT-F, proxy ESSPRI scores and physician reported severity between patients with differing time to diagnosis (Table 2), assessed at the time of consultation. Relationships between diagnosis duration and WPAI scores were not statistically significant.
Conclusion: Delayed diagnosis of pSS is associated with poorer patient outcomes; including worsening PRO scores, and ESSPRI scores. pSS diagnosis periods could likely be attenuated by increasing disease awareness amongst physicians; thus improving patient outcomes in pSS.
To cite this abstract in AMA style:
Ndife B, Barlow S, Hughes M, Booth N. The Impact of Delayed Primary Sjögren’s Syndrome Diagnosis on Patient Outcomes: A Real-World Survey in the US [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/the-impact-of-delayed-primary-sjogrens-syndrome-diagnosis-on-patient-outcomes-a-real-world-survey-in-the-us/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-impact-of-delayed-primary-sjogrens-syndrome-diagnosis-on-patient-outcomes-a-real-world-survey-in-the-us/