Session Information
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: The COVID19 pandemic was a turning point for Rheumatology. This survey of rheumatologists (rheums) assessed its impact on care delivery, patient counseling and drug use in the first 3 months of the pandemic.
Methods: 2406 rheums were surveyed by email in June 2020. The 26 questions assessed respondent demographics, geography, practice type, care delivery, counseling, risks and prevalence of COVID in rheumatic disease (RMD) patients (pts).
Results: 400 responses (16.7%) were received. Average respondent age was 54 yrs, 61% male, in practice for 21 years, avg 67 pts seen per week; most were in private practice (group 27%, solo 27%, multispecialty 22%) or academics (24%). 5% of respondents practiced outside the US.
Care Delivery: Figure 1 shows substantial reductions in number of new pt visits (64%), hospital consults (56%), follow-ups visits (55%), joint injections (55%), urgent (49%) and research visits (42%). Major service increases were seen in telehealth ( >75%) visits. Many noted < 20% patients had no telemedicine access. Rheums temporarily closed their clinics, for either 4 weeks (32%), 6-8wks (28%) or 12 wks (14%); 19% have still not reopened. A major disruption to practice was noted by 46% rheums; 4% had no change. A major income loss was claimed by 31%, and 17% had no income loss.
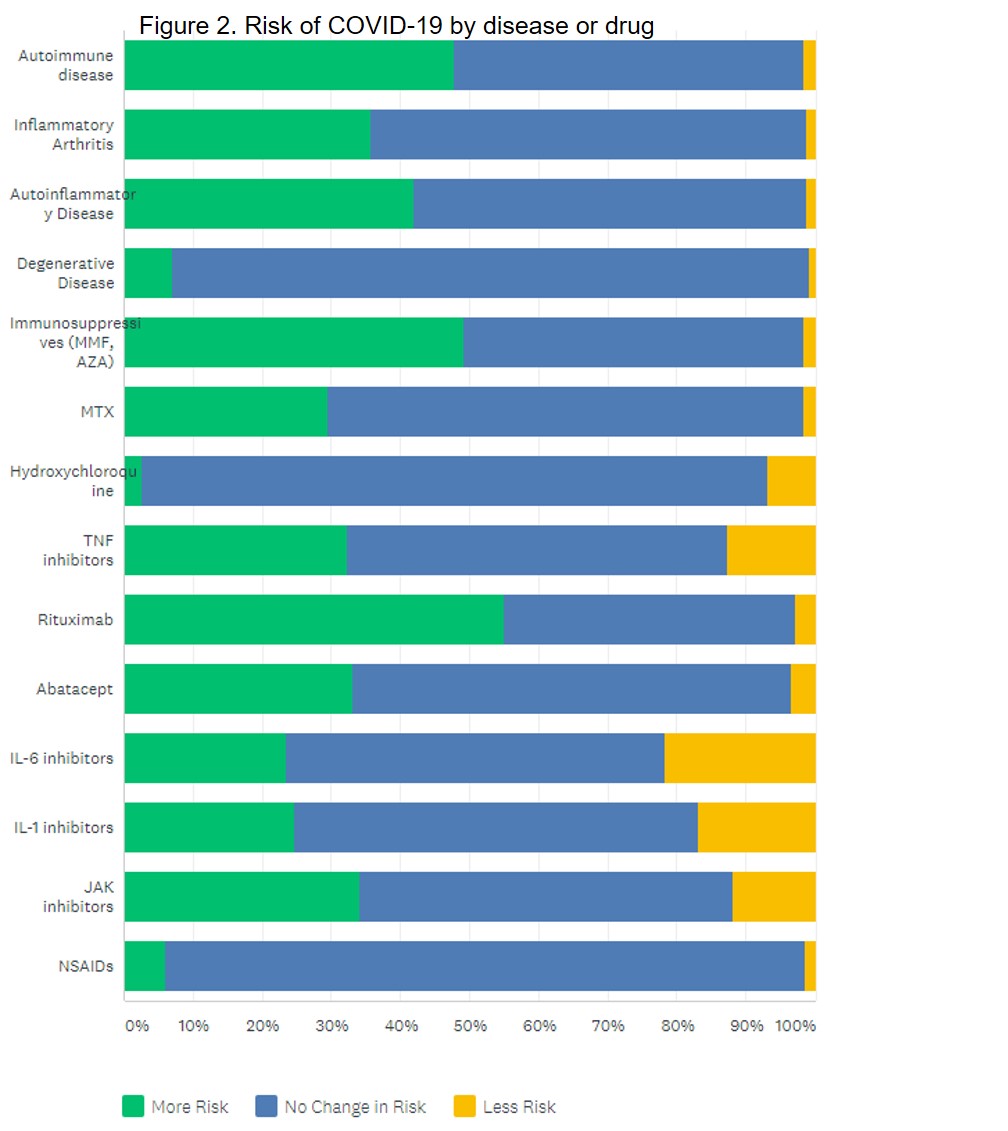
Patient Counseling: 40% rheums noted ongoing patient confusion about COVID. Two-thirds informed pts their disease does NOT increase COVID risk. RA & SLE pts were told risk is not higher if they are well controlled on stable meds (27%) or that risk was due to comorbidities & age (21%); rather than meds (9%). Majority noted no COVID risk imposed by NSAIDs (93%), OA (92%), HCQ (91%), MTX (69%), abatacept (64%) or inflammatory arthritis (63%). Rheums suggested an increased risk with rituximab (55%), immunosuppressives (49%) or active autoimmune disease (47%). Rheums perceptions of COVID risk are shown in Figure 2.
Prescribing Habits: Overall, rheums did not change their use of NSAIDs, MTX, HCQ, TNF inhibitors abatacept, IL-6 inhibitors, or MMF. Prednisone use decreased 41%, as did rituximab 26%, cyclophosphamide 19% and denosumab 18%; antidepressants (9%) and hydroxychloroquine (7%) increased. Nearly all rheums (94%) said <25% of patients reduced or discontinued meds without seeking advice. 10% prescribed antimalarials as COVID prophylaxis, and 82% of rheums reported patients had difficulty getting antimalarials (shortages/cost issues).
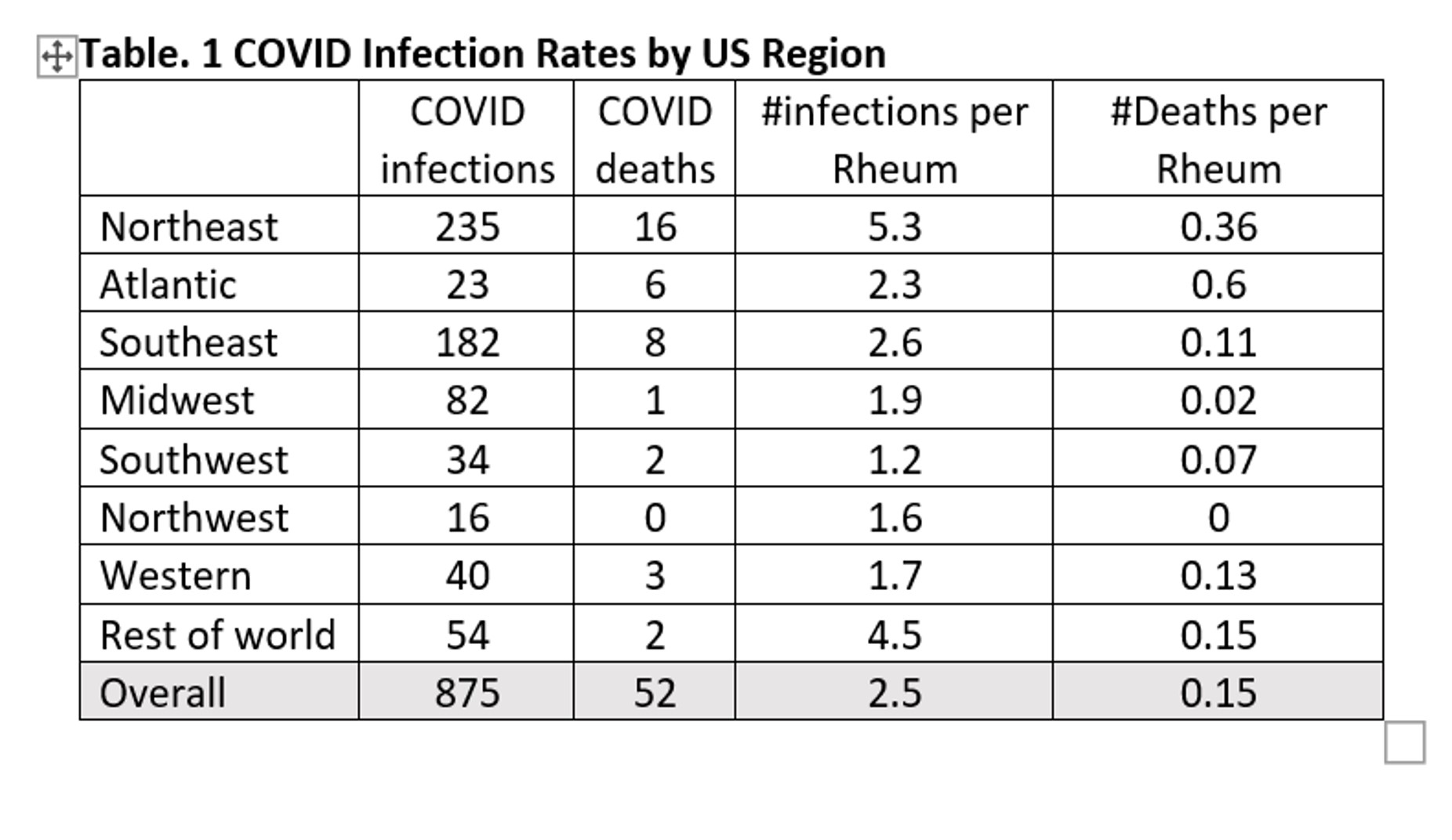
Rheums Role: Most (61%) have not been involved in COVID-19 care, while 30% were consulted about DMARD/biologics; only 6% have managed cytokine storm (CSS). The preferred agent for CSS was IL-6 inhibitor (66%), and 14% did not know what to use. A total of 348 rheums reported 875 cases of COVID, (2.51 patients/Rheum). With an average Rheum patient panel of 1350 patients, the COVID infection rate was 0.18% in RMD pts. Total of 52 deaths were reported, with a COVID death rate of 0.01% in RMD patients.
Conclusion: Rheums substantially changed their practices, counseling and health care delivery during the pandemic. COVID infection and death rates among RMD patients appears to be lower than the general US population. Maintenance of drug therapy and patient compliance appears potentially protective to SARS-CoV-2.
To cite this abstract in AMA style:
Bacalao M, Dao K, Cush J. The Evolution of Rheumatologist’s Practice in Response to the COVID19 Pandemic [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/the-evolution-of-rheumatologists-practice-in-response-to-the-covid19-pandemic/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-evolution-of-rheumatologists-practice-in-response-to-the-covid19-pandemic/