Session Information
Date: Sunday, November 12, 2023
Title: (0609–0672) Systemic Sclerosis & Related Disorders – Clinical Poster I: Research
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: The occurrence of lower limbs macrovascular complications configuring lower extremities arterial disease (LEAD) has been reported in Systemic Sclerosis (SSc) patients. Recently, digital ulcers (DUs), pulmonary arterial hypertension (PAH), steroid use and active smoking/having stopped ≤3 years were identified as factors associated with lower limbs amputation in a single-centre SSc cohort1. Our aim was the estimation of LEAD prevalence in: (i) the overall SSc cohort and (ii) at-risk patients according to the above-mentioned features.
Methods: Consecutive SSc patients attending our centre for scheduled visits between October 2022 and April 2023 were included. Patients without known LEAD with ≥1 feature associated to lower limb amputation, as described above1 were referred for lower extremities arterial Doppler ultrasonography (DUS) performed by a single expert vascular surgeon.
Results: Among 192 SSc patients evaluated (93% females, 81% limited cutaneous involvement, 45% anti-centromere), 18 (9%) were previously diagnosed with LEAD, requiring revascularization interventions in 8 (44%) and amputations in 5 (28%). As compared to the remaining 174, they were older (median[1st-3rd quartile]: 75[69-79] vs 62[51-70] years; p< 0.001), had a longer disease duration (20[15-27] vs 12[6-19] years; p:0.004), higher frequency of DUs (90% vs 54%; p:0.001), especially at lower limbs (67% vs 12%; p< 0.001), more comorbidities (Charlson Comorbidity Index: 6[5-7] vs 3[2-5]; p< 0.001), and were more frequently treated with prostanoids (67% vs 31%; p:0.002) and steroids (61% vs 31%; p:0.010).
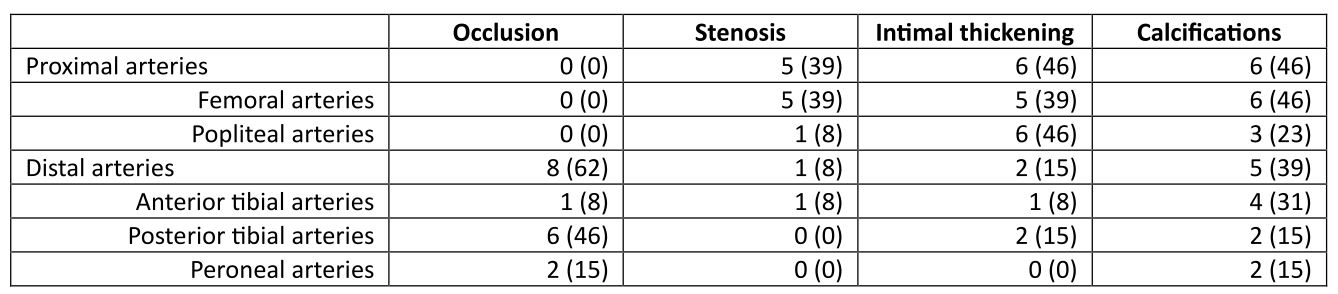
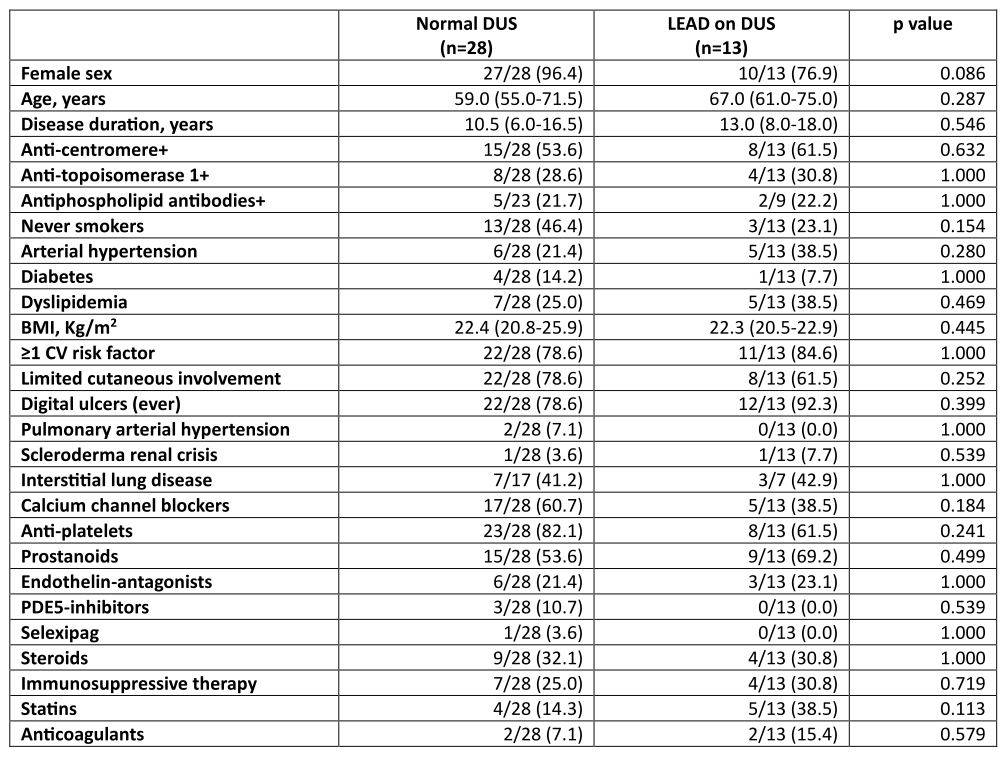
At least 1 LEAD risk factor was identified in 124/174 patients (71%) (DUs (77%); steroid use (40%); smoking (26%); PAH (5%)). Among 41 patients so far evaluated by DUS, LEAD was detected in 13 (32%) (Table 1): 10 were asymptomatic (stage I), 2 reported mild claudication (stage IIa), 1 reported pain also at rest (stage III). 10/13 were already on treatment with anti-platelets/anti-coagulants, in the remaining 3 patients low dose aspirin was added; the patient with LEAD stage III was referred to angiographic study. As compared to 28 patients with a normal DUS, no differences were observed in clinical-demographic features (Table 2).
Conclusion: Based on these preliminary data, in our SSc cohort the prevalence of diagnosed LEAD stands at 9%. However, by selecting at-risk SSc patients (DUs, PAH, steroid use and smoking), LEAD signs on DUS were detected in 32% of them, mostly free from lower limb symptoms and traditional CV risk-factors. This underlines the need to implement the diagnostic/therapeutic work-up of SSc patients by performing lower extremities arterial DUS and including vascular surgeons in the multidisciplinary team dedicated to SSc patients.
References. 1Bertolino et al. JSRD. 2020
The Authors would like to thank GILS Patient Association for kindly supporting this project.
Abbreviations: BMI= Body Mass Index, CV= cardiovascular, PDE5= phosphodiesterase 5.
To cite this abstract in AMA style:
Lazzaroni M, Moschetti L, Pedretti E, Baggi P, Franceschini F, Bonardelli S, Airò P. The Evaluation of Lower Extremities Arterial Disease in Systemic Sclerosis Patients Through Rheumatologist-Vascular Surgeon Multidisciplinary Management: Preliminary Data from an Italian Single Center Study [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/the-evaluation-of-lower-extremities-arterial-disease-in-systemic-sclerosis-patients-through-rheumatologist-vascular-surgeon-multidisciplinary-management-preliminary-data-from-an-italian-single-center/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-evaluation-of-lower-extremities-arterial-disease-in-systemic-sclerosis-patients-through-rheumatologist-vascular-surgeon-multidisciplinary-management-preliminary-data-from-an-italian-single-center/