Session Information
Session Type: Poster Session D
Session Time: 1:00PM-3:00PM
Background/Purpose: The concept of treat-to-target (T2T), a strategy in which treatment is directed to reach and maintain a defined goal such as remission or low disease activity (LDA), has been utilised to care of rheumatic diseases since ~2010. This systematic review and meta-analysis aims to comprehensively evaluate the evidence of the effectiveness of a T2T strategy in the management of rheumatic diseases.
Methods: A systematic literature search was performed across all types of rheumatic diseases to identify studies where (i) a T2T strategy was compared with usual care (UC), or (ii) a T2T strategy was evaluated, albeit without a comparison arm, in the real world. Clinical, functional, and radiologic outcomes, cost-effectiveness, and adverse events (AEs) of the T2T strategy were reviewed and random-effect meta-analyses were conducted.
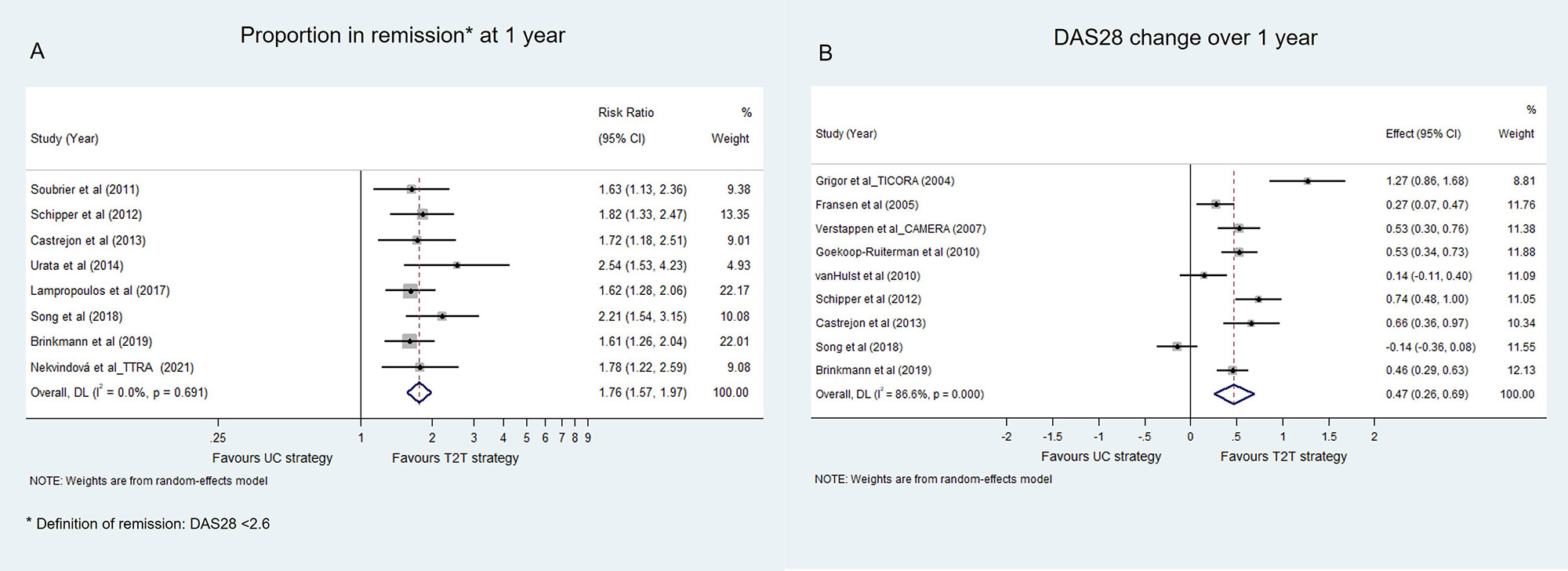
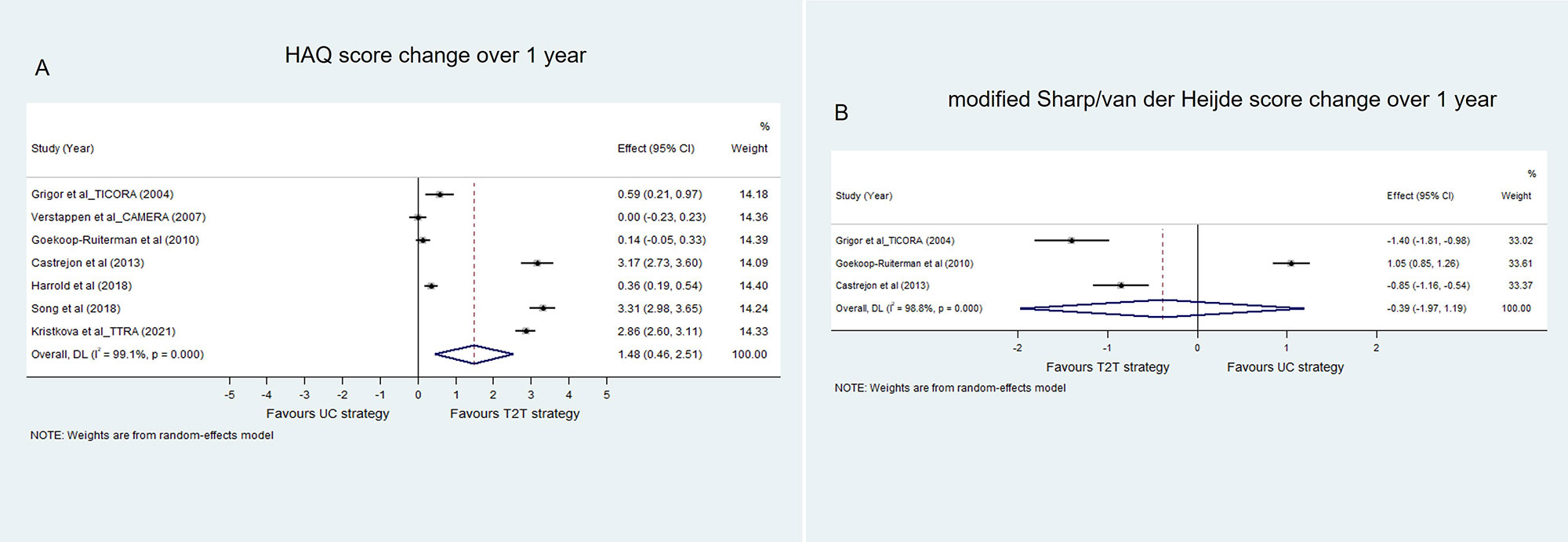
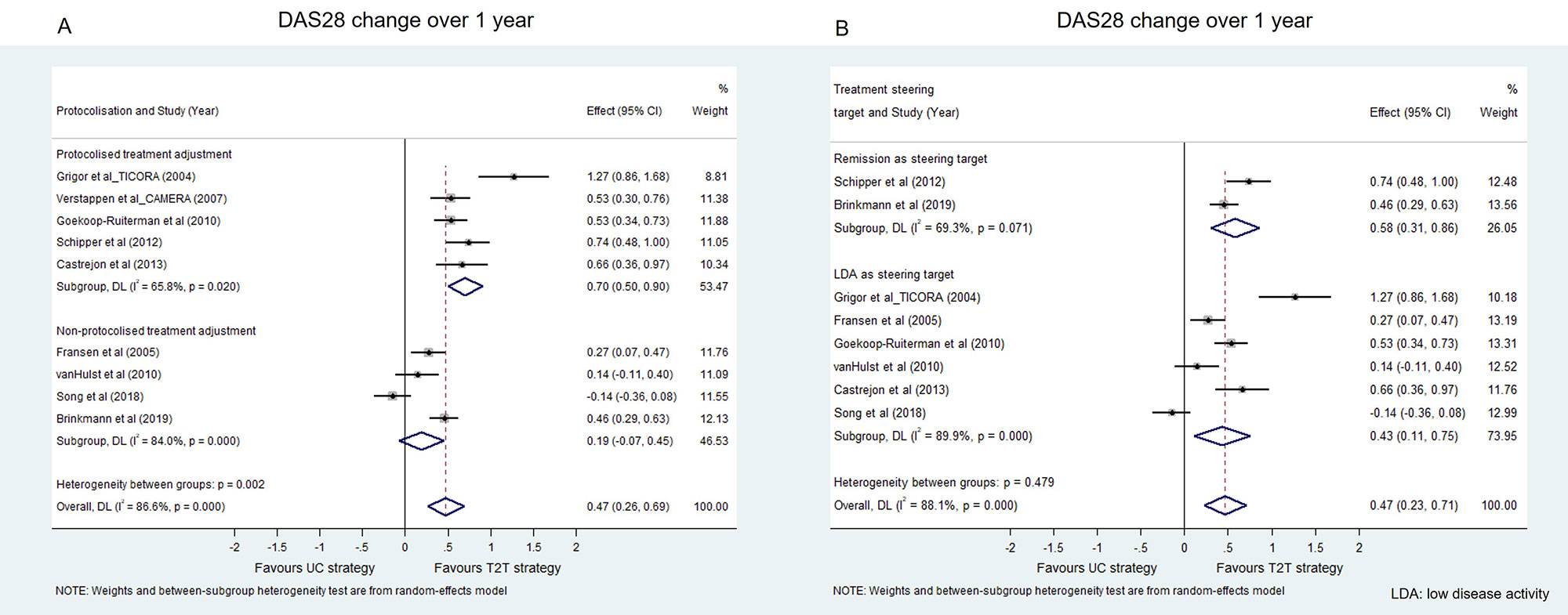
Results: Twenty-six comparative (T2T strategy versus UC) studies (22 in RA, 3 in PsA and 1 in SpA) and 11 non-comparative real-world studies in RA were included in the analyses. Most studies (97%, 36/37) recruited patients with active disease. Compared with UC, T2T strategy was shown in 86% (19/22) of RA studies to have a better clinical outcome. The meta-analyses for both remission rate (pooled risk ratio: 1.76 [1.57-1.97], p=0.000, Figure 1A) and DAS-28 change (pooled standardised mean difference (SMD): 0.47 [0.26-0.69], P=0.000, Figure 1B) over 1 year favoured a T2T strategy. In terms of the physical function outcome, the pooled result of HAQ score change over 1 year also favoured a T2T strategy (pooled SMD 1.48 [0.46-2.51], p=0.004) (Figure 2A). However, the pooled result of modified total Sharp/van der Heijde score change over 1 year from 3 studies did not show a significant difference between the T2T strategy and UC (Figure 2B). Two out of two studies found the T2T strategy was more cost-effective than UC and 6 out of 6 studies showed no increased AEs T2T strategy compared to UC. A sensitivity analysis showed that a T2T strategy with a predefined treatment protocol had better clinical effectiveness compared with a T2T strategy without protocol (pooled SMD 0.70 [0.50-0.90] vs 0.19 [-0.07-0.45], Figure 3A). As a treatment steering target, LDA showed a comparable clinical benefit with remission (pooled SMD 0.43 [0.11-0.75] vs 0.58 [0.31-0.86], Figure 3B). For the non-comparative studies, the pooled remission rates at 1, 3 and 5 years with a T2T strategy were 50% (36%-64%), 57% (48%-67%) and 64% (60%-68%), respectively. For the studies in PsA and SpA, the T2T strategy was also more effective than UC in clinical and physical function outcomes, but not in radiologic outcomes.
Conclusion: For patients with active RA, a T2T strategy has shown advantages in increasing clinical response and improving physical function without significantly increasing costs and AEs and is feasible and effective to apply in the real world. A predefined treatment protocol is more beneficial in terms of clinical response than an ad hoc approach to target driven treatment. A limited number of studies have also shown clinical benefits from T2T strategies in active PsA and SpA patients. There were no T2T strategy studies in other rheumatic diseases, highlighting an urgent unmet need.
To cite this abstract in AMA style:
Hao Y, Oon S, Nikpour M. The Effectiveness of a Treat-to-target Strategy in Rheumatic Diseases: A Systematic Literature Review and Meta-analysis [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/the-effectiveness-of-a-treat-to-target-strategy-in-rheumatic-diseases-a-systematic-literature-review-and-meta-analysis/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-effectiveness-of-a-treat-to-target-strategy-in-rheumatic-diseases-a-systematic-literature-review-and-meta-analysis/