Session Information
Session Type: ACR Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose:
Prescribing the first biologic for rheumatoid arthritis is an important decision for physicians, payers, and patients with costs and clinical implications. Our aim was to describe disparities in access to the first biologic prescribed to patients with rheumatoid arthritis in a single payer health care system (no insurance confounders) to explain the relative contributions of patient, prescriber and geographic region characteristics to receipt of first biologic.
Methods:
Our study design is a population retrospective administrative data-based population study conducted in Ontario Canada. We used a time-series analysis to describe trends in rheumatologist preference and nested Cox proportional hazards models with random effects and time varying exposures to adjust for patient, physician and geographic area characteristics. Patients had an incident RA diagnosis between 2001 to 2015 after 66 years of age in Ontario Canada and received at least one csDMARD or biologic. The main exposure was time from the first csDMARD prescription to the outcome of first biologic prescription, adjusted for patient, prescriber and geographic area variables. Patient covariates were age, sex, disease duration, socioeconomic status, distance to care and supply of care in the patient’s area of residence. Prescriber covariates were year of graduation, specialty of practice, and the supply of rheumatologic care in the patient’s geographic region. Patients were censored at death, move out of province or end of study follow-up.
Results:
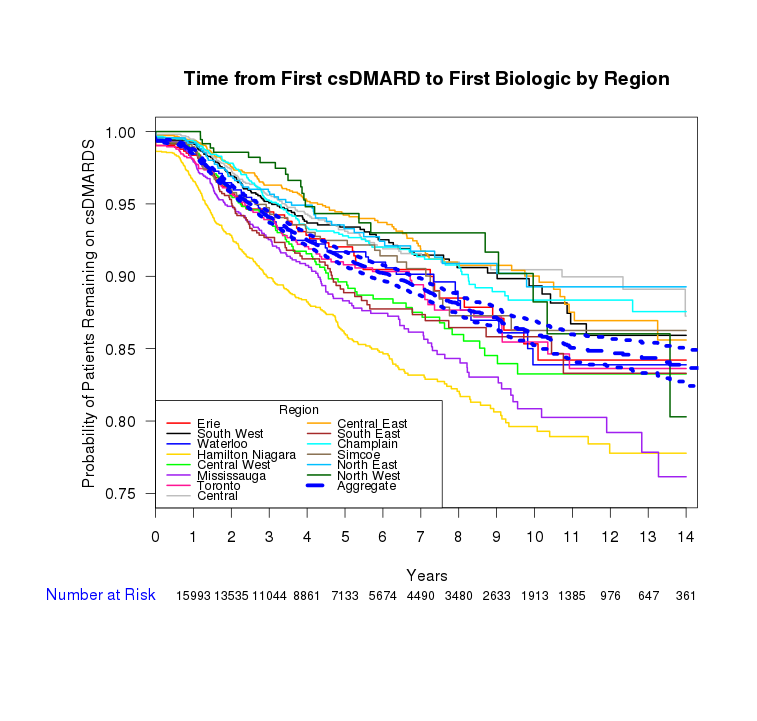
A total of 17,672 patients met the study inclusion criteria accruing 82,445.79 patient-years of follow up. Variables significantly associated with delayed receipt of first biologic medication, were older age, sex (male) (HR=0.76), lower socioeconomic status (HR=0.92), greater distance to nearest rheumatologist (HR=0.95). Rheumatologist preference for and use of biologics increased 2.5-fold in the study time period but have not kept pace with the number of new active RA patients (3 fold). Geographic area level differences in time to prescriptions of first biologic exists and widens over time with about a 10% difference from highest to lowest prescribing regions 2 years after first csDMARD prescription (Figure 1). Prescriber preference (after adjustment for patient and physician covariates) accounted for 65% of prescription variation while differences between the regions themselves contributed 4.6% to the overall prescription variation.
Conclusion:
From a direct measurement of the total Provincial population of RA patients with identical medication coverage, variation in time to receipt of first biologic exist after adjusting for individual level patient, prescriber, and geographic area covariates. These findings illustrate systemic gaps in care and the influence of physician preferences that could be further optimized to improve patient outcomes.
To cite this abstract in AMA style:
Tatangelo M, Tomlinson GA, Paterson M, Bansback N, Gomes T, Kopp A, Ahluwalia V, Bombardier C. The Effect of Patient, Prescriber and Region on the Initiation of First Biologic for Rheumatoid Arthritis: A Longitudinal Population Study [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/the-effect-of-patient-prescriber-and-region-on-the-initiation-of-first-biologic-for-rheumatoid-arthritis-a-longitudinal-population-study/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-effect-of-patient-prescriber-and-region-on-the-initiation-of-first-biologic-for-rheumatoid-arthritis-a-longitudinal-population-study/