Session Information
Date: Friday, November 6, 2020
Title: RA – Diagnosis, Manifestations, & Outcomes Poster I: Multimorbidity
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Patients with elderly onset rheumatoid arthritis(RA) have been reported to be less positive for RF(rheumatoid factor) and ACPA(anti-cyclic citrullinated peptide antibody), and have a higher risk of malignancy than young onset RA. The aim of this study was to investigate the relationship between seronegative RA and malignancy, and to examine the clinical and laboratory features of those with and without malignancy.
Methods:
We retrospectively examined consecutive patients diagnosed with seronegative RA in our hospital from 2007 to 2019. Patients with seronegative RA were negative for both RF and ACPA and met the EULAR/ACR 2010 criteria. The patients who were diagnosed with remitting seronegative symmetrical synovitis with pitting edema syndrome or polymyalgia rheumatica at first and then diagnosed with seronegative RA afterward were included in seronegative RA. The first analysis was performed on the affected joints, C-reactive protein(CRP), erythrocyte sedimentation rate(ESR), hemoglobin(Hb), albmin(Alb), immunoglobulin G(IgG), fibrinogen, lactate dehydrogenase(LDH), matrix metalloproteinase 3(MMP-3), image findings(ultrasound, X-ray, and MRI), and the history of malignancy 2 years before and after the diagnosis with seronegative RA. The affected joints were large joints(shoulders, elbows, hips, knees, and ankles), wrists, finger joints (MCP, and PIP joints), and toe joints (MTP and PIP joints). The secondary analysis was performed on the above evaluations with a propensity score (PS) matching for sex.
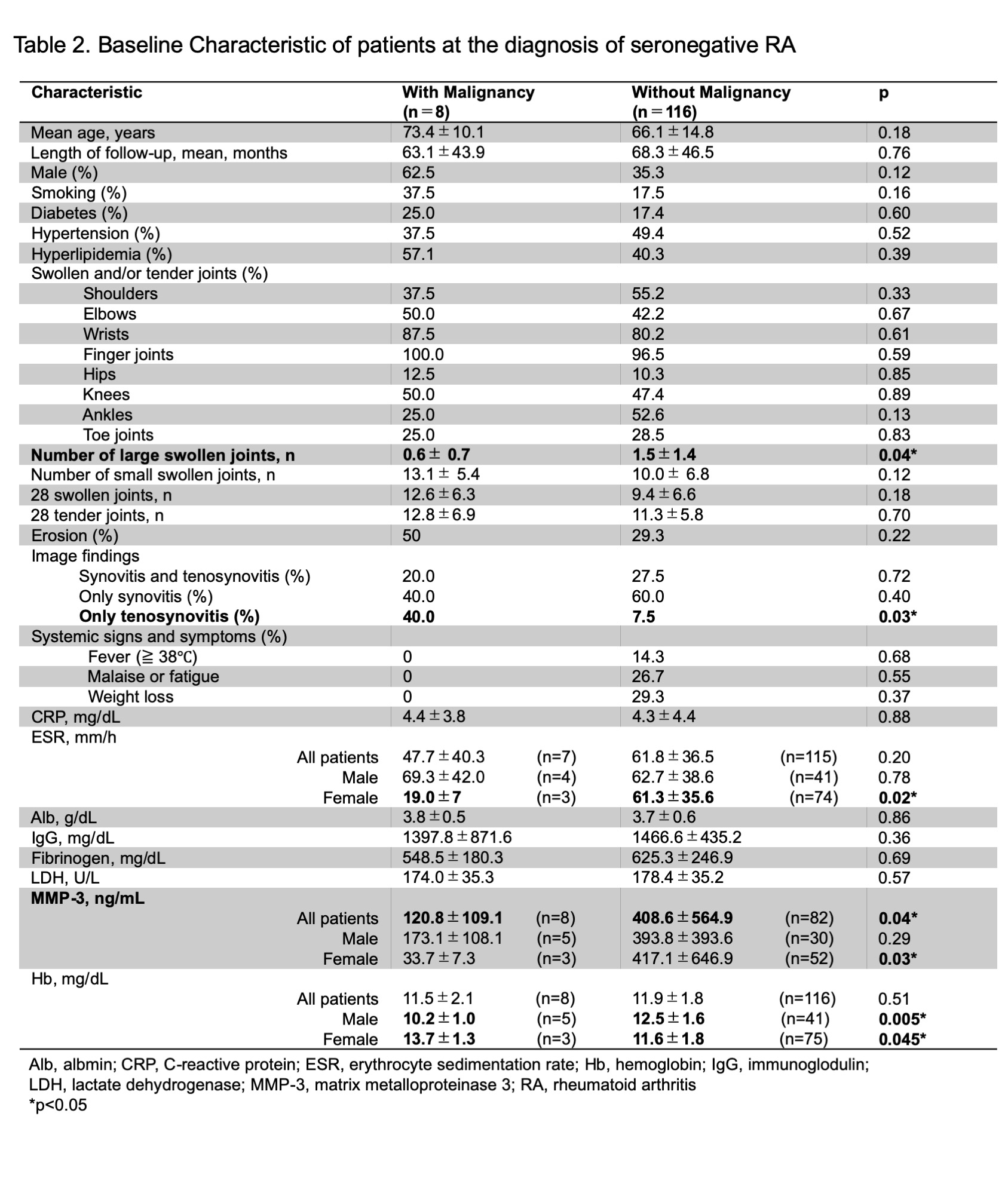
Results: In the first analysis, 124 patients with seronegative RA were enrolled. Eight patients had malignancies, and 116 patients did not have malignancy. Table 1 shows the types of malignancy. The median time for the diagnosis of malignancy was 10 months after the diagnosis of RA. Table 2 shows the baseline characteristics at the diagnosis of seronegative RA. The mean ages with and without malignancy were 73.4±10.1 and 66.1±14.8 years old, respectively(p= 0.18). Males were 62.5% and 35.3%(p=0.12). The mean numbers of large swollen joints were 0.6± 0.7, 1.5±1.4(p=0.04). There was no difference in the levels of CRP, ESR, Hb, Alb, IgG, fibrinogen, LDH between seronegative RA with and without malignancy. The levels of MMP-3 were 120.8±109.1 and 408.6±564.9 ng/mL(p=0.04). The patients with only tenosynovitis were 40.0% and 7.5%(p=0.03).
In the secondary analysis with PS, 8 patients with malignancy and 8 patients without malignancy were enrolled(Table 3). The mean numbers of large swollen joints were 0.6± 0.7, 1.5±1.4(p=0.04). The mean levels of MMP-3 were 120.8±127.1 and 425.8±127.1 ng/mL (p=0.07).
Conclusion: In seronegative RA, the patients with malignancy had lower levels of MMP-3 and fewer numbers of large swollen joints at the time of RA diagnosis than those without malignancy. The patients with only tenosynovitis were more common in the patients with malignancy than in those without malignancy. Furthermore, among seronegative RA patients, it was considered that the patients with lower levels of MMP-3 and fewer numbers of large swollen joints should pay attention especially to the complication of malignancy.
To cite this abstract in AMA style:
Higashida-Konishi M, Izumi K, Hama S, Takei H, Okano Y, Ohshima H. The Clinical and Laboratory Features of Seronegative Rheumatoid Arthritis with and Without Malignancy [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/the-clinical-and-laboratory-features-of-seronegative-rheumatoid-arthritis-with-and-without-malignancy/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-clinical-and-laboratory-features-of-seronegative-rheumatoid-arthritis-with-and-without-malignancy/