Session Information
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Knowledge gaps exist regarding time-trends for the main causes (Cardiac/renal disease vs. infections) hospitalizations in gout. Therefore, we examined whether specific causes (cardiovascular, renal, musculoskeletal, pulmonary, infection) of non-gout hospitalizations and mortality, have changed over time in people with gout.
Methods: We used the U.S. National Inpatient Sample (NIS) data from 1998 to 2014, the last calendar year with International Classification of Diseases, ninth revision, clinical modification (ICD-9-CM) in the U.S. NIS represents a 20% stratified sample of discharges for the U.S., a part of the Agency for Healthcare Research and Quality’s (AHRQ) healthcare cost and utilization project (HCUP).
Our study cohort included people hospitalized with a secondary diagnosis of gout based on an ICD-9-CM code, 274.xx, a valid approach with high sensitivity (90%), specificity (100%) and positive predictive value (80%). We assessed whether the rank (and % hospitalizations) of specific diseases in the top 25 Clinical Classifications Software (CCS; and top 5) categories associated with hospitalizations in gout changed between the first (1998-99) and the last study periods (2013-14). CCS is a tool for clustering patient diagnoses and procedures (primary or secondary) into manageable clinically meaningful categories [5]. We chose 2014 as the last study year, due to switching from ICD-9-CM to ICD-10-CM in 2015.
Results: Non-gout Hospitalizations in people with gout: There were 501,847 non-gout hospitalizations in 1998-99 and 1,665,355 in 2013-14. The top four CCS categories did not change rank from 1998-99 to 2013-14, but both top 2-ranked categories, circulatory system and heart diseases, decreased by 9-10%. Infection categories increased from three in the top 25 CCS categories in 1998-99 (rank # 11, 15 and 20) to five in 2013-14 (rank #10, 11, 12, 18 and 21; Figure 1A), and included pneumonia, respiratory infections, infections/parasitic diseases and sepsis. Musculoskeletal diseases were rank #5 for hospitalization in 2013-14 and osteoarthritis was also newly added to the top 25 ranks for non-gout hospitalizations.
In-hospital mortality: Circulatory system disease was rank #1 in both in 1998-99 and 2013-14, but the attributed proportion decreased from 40% to 29%. Two infection categories were in the top ten in 1998-99 (respiratory infection, rank #7; pneumonia, rank #8) versus four infection categories in the top five CCS categories in 2013-14 (rank #2, #3, #4 and #5; Figure 1B). Most cardiac diseases and neoplasms were less frequent, while infection, respiratory failure, renal disease were more frequent in 2013-14 (Figure 1B).
Conclusion:
Non-gout hospitalizations in people with gout increased over 2-decades. In-hospital mortality in patients with gout showed a replacement of cardiac/respiratory causes in ranks #2-5 in 1998-99 by infectious disease/sepsis in 2013-14. Cardiovascular diseases were the main reasons for non-gout hospitalizations in people with gout in both periods; but more importantly, their relative contribution decreased over 2-decades, while relative contributions of infectious and musculoskeletal diseases (including osteoarthritis) increased.
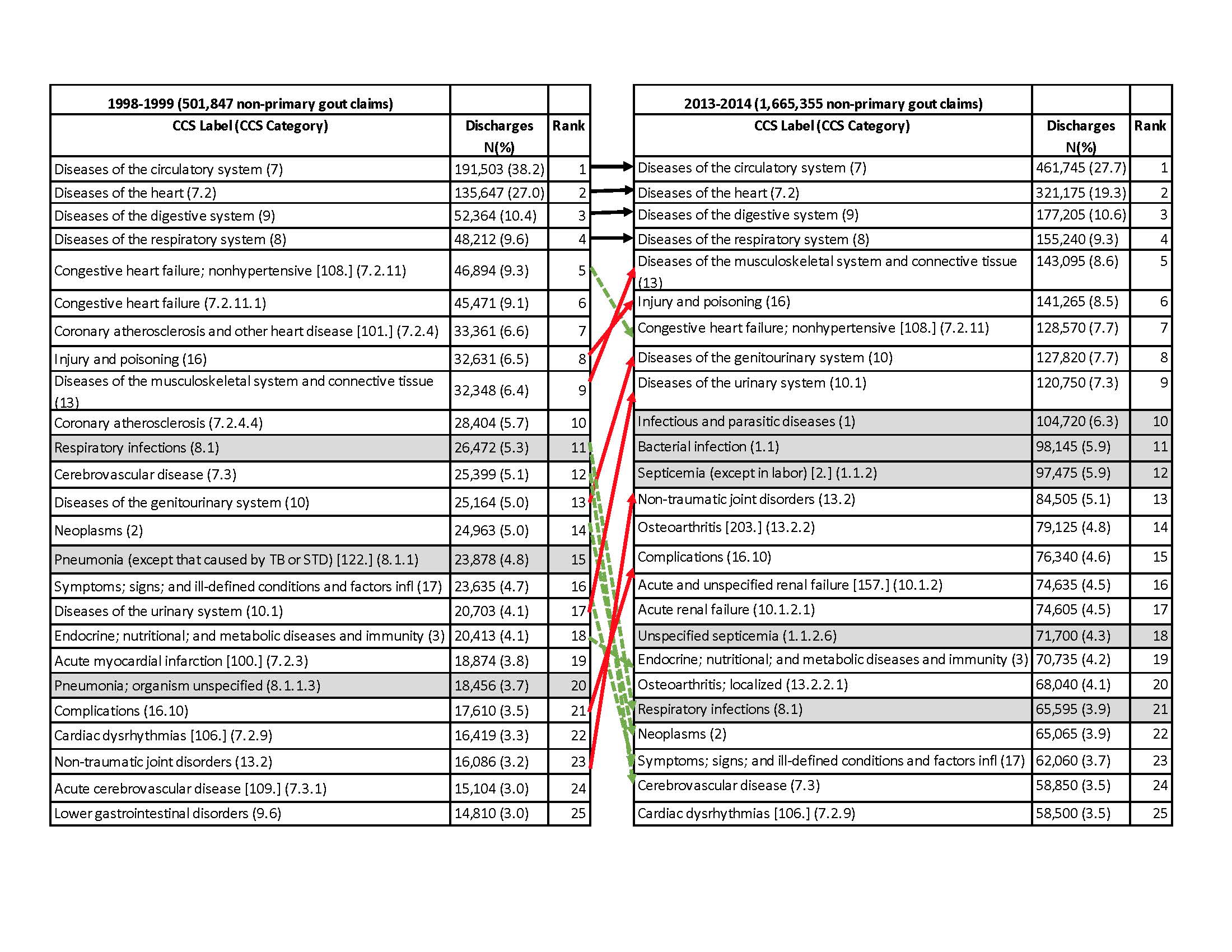 Figure 1. Top 25 healthcare cost and utilization project (HCUP) Clinical Classifications Software (CCS) category ranks based on diagnosis or procedures for hospitalizations (1A) and in-hospital death (1B) in people with gout comparing the first study (1998-1999) to the last study period (2013-2014) Figure 1 legend. Solid red arrows show the categories whose rank increased from 1998-1999 to 2013-2014, dashed green arrows whose rank decreased and solid black arrows with the same rank. Each CCS category label and category are shown in the first column. Square brackets refer to single-level CCS categories and regular brackets refer to multi-level CCS categories.
Figure 1. Top 25 healthcare cost and utilization project (HCUP) Clinical Classifications Software (CCS) category ranks based on diagnosis or procedures for hospitalizations (1A) and in-hospital death (1B) in people with gout comparing the first study (1998-1999) to the last study period (2013-2014) Figure 1 legend. Solid red arrows show the categories whose rank increased from 1998-1999 to 2013-2014, dashed green arrows whose rank decreased and solid black arrows with the same rank. Each CCS category label and category are shown in the first column. Square brackets refer to single-level CCS categories and regular brackets refer to multi-level CCS categories.
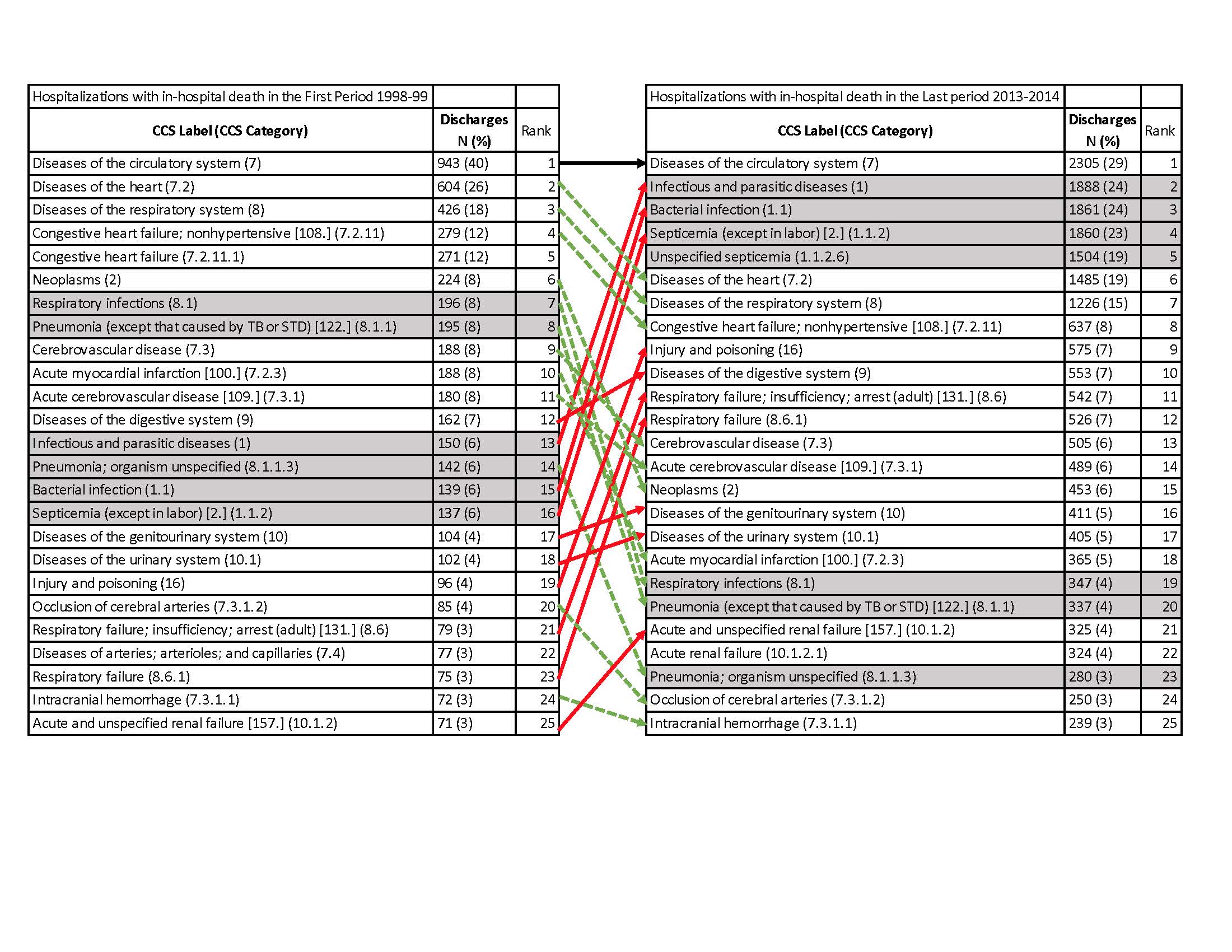 Figure 1B. See title and legend with the panel above
Figure 1B. See title and legend with the panel above
To cite this abstract in AMA style:
Singh J, Cleveland J. The Changing Epidemiology of Inpatient Gout and Associated Mortality: A 17-year National Study [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/the-changing-epidemiology-of-inpatient-gout-and-associated-mortality-a-17-year-national-study/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-changing-epidemiology-of-inpatient-gout-and-associated-mortality-a-17-year-national-study/
