Session Information
Session Type: Abstract Session
Session Time: 3:30PM-3:45PM
Background/Purpose: Systemic Lupus Erythematosus (SLE) is a chronic immune-mediated disease with 20-25% patients needing hospital admission annually. Early readmissions add to the clinical and economic burden on the healthcare system. Strategies to reduce readmission are now a crucial aspect of management. Therefore, we conducted this study to investigate the outcomes and predictors of 30-day readmission in patients with SLE.
Methods: We queried the 2017 Nationwide Readmission Database (NRD) using ICD-10-CM diagnosis codes to identify all patients admitted with a primary diagnosis of SLE. Outcomes assessed were 30-day readmission rates, mortality, length of stay (LOS) and hospitalization costs. A multivariate cox regression was done to obtain Hazard Ratio (HR) and identify independent predictors of readmission. Statistical analysis was performed using STATA software.
Results: A total of 8,664 adult patients were admitted with a primary diagnosis of SLE in 2017, with in-hospital mortality rate of 0.87%. Of the patients discharged, 23.72% patients were readmitted within 30-days. The most common primary diagnosis at readmission was “Systemic lupus erythematosus, unspecified” (12.99%). When compared to index admission, readmitted patients had higher in-hospital mortality (3.16% vs 0.87%, p< 0.01), longer mean LOS (7.05 days vs 6.4 days, p< 0.05) and higher mean hospitalization charges ( $76,055 vs $68,087, p< 0.01). Readmissions added 14,427 inpatient days and $36 million in hospitalization cost to the healthcare burden. Higher Charlson comorbidity score (HR 1.08, p< 0.01), CHF (HR 1.36, p< 0.01), AKI (HR 1.24, p< 0.01), CKD (HR 1.32, p< 0.01), ESRD (HR 1.29, p< 0.01), and discharge other than home discharge (HR 1.36, p< 0.01) were independently associated with increased likelihood of 30-day readmission.
Conclusion: We performed a comprehensive assessment of patients admitted with SLE with the national inpatient data using the newer specific ICD-10 codes. In the US, about 1 in 4 patients with SLE are readmitted within 30-days of discharge. Readmission is associated with significantly increased in-hospital mortality, LOS, and hospitalization costs. 30-day readmissions resulted in an increased burden to healthcare resource utilization, adding considerable in-patient stay days and hospitalization costs. Patients with AKI, CHF, CKD, ESRD, discharge other than home discharge and higher comorbidity burden were significantly more likely to be readmitted within 30-days. Further prospective studies are needed to assess the high-risk populations to reduce early readmission and improve value-based care.
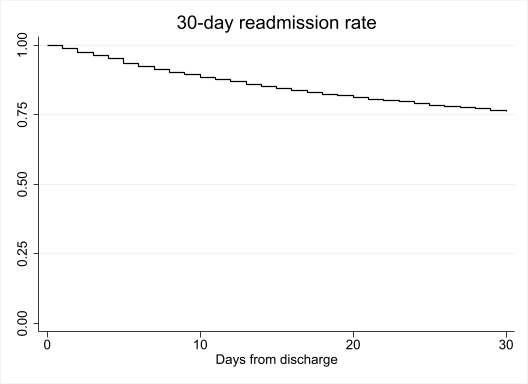 KM graph of 30-day readmission
KM graph of 30-day readmission
To cite this abstract in AMA style:
Acharya A, Iftikhar S, Khader Y, Sharma S, Gekonde J, Fatima R, Burmeister C, Altorok N. The Burden of Thirty-day Readmission and Independent Predictors of Readmission in Patients with Systemic Lupus Erythematosus: A Nationwide Analysis [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/the-burden-of-thirty-day-readmission-and-independent-predictors-of-readmission-in-patients-with-systemic-lupus-erythematosus-a-nationwide-analysis/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-burden-of-thirty-day-readmission-and-independent-predictors-of-readmission-in-patients-with-systemic-lupus-erythematosus-a-nationwide-analysis/
