Session Information
Session Type: Poster Session (Sunday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Rheumatoid arthritis (RA), psoriatic arthritis (PSA) and spondyloarthritis (SPA) are the most common inflammatory rheumatic diseases, associated with a high burden of comorbidities and polypharmacy, especially analgesics. Thus, we compared comorbidity burden and usage of pain-related medication in patient with RA, PSA and SPA versus controls in a general practitioner (GP) setting.
Methods: Data over a 13-year time interval (1999-2012) were obtained from a Flemish GP-based morbidity registration network, called Intego that covers 2% of the Flemish general population. Patients classified on the International Classification of Primary Care (ICPC) codes L88 (rheumatoid/seropositive arthritis) and L99 (musculoskeletal disease other) were selected for this study. Experienced rheumatologists verified if the codes corresponded to a diagnosis of RA/SPA/PSA. Diagnosis date in Intego was considered “baseline”. Per case, 4 controls were selected from all other ICPC codes and matched with cases by age, gender, GP practice, and date of diagnosis. The total comorbidity burden was summarised by calculating the Rheumatic Disease Comorbidity Index (RDCI) score at baseline and after 3 years. RDCI ranges from 0-9, with 9 being the highest comorbidity burden. Incidence rates of comorbidities included in this index were calculated. Prevalent analgesic medication use in RA/SPA/PSA patients versus controls was determined. Mann Whitney and χ2 tests were used when appropriate.
Results: Over the 13-year period, 738, 229 and 167 patients were included with a diagnosis of RA (mean(SD) age 57.7(17.2), 68% female), SPA (mean(SD) age 40.6(15.1), 50% female) and PSA (mean(SD) age of 47(13.2), 48% female), respectively.
The mean(SD) RDCI at baseline was 1.2(1.4), 0.6(1.0) and 1.0(1.3) for RA, SPA or PSA respectively. After 3 years, the mean(SD) RDCI was 1.5(1.6), 0.8(1.2) and 1.3(1.4) for RA, SPA or PSA respectively. The RDCI differed after 3 years between RA and controls (1.5(1.6) versus 1.4(1.5), p=0.008), and PSA and controls (1.3(1.4) versus 1.0(1.4), p=0.009). In RA, at baseline 58% of individuals had an RDCI score ≥1 (versus 53% controls, p=0.01) and after 3 years, 66% of individuals had an RDCI score ≥1 (versus 60% controls, p=0.004). In SPA, at baseline 36% of individuals had an RDCI score ≥1 (versus 34% controls, p=0.6) and after 3 years, 45% of individuals had an RDCI score ≥1 (versus 41% controls, p=0.4). In PSA, at baseline 52% of individuals had an RDCI score ≥1 (versus 42% controls, p=0.03) and after 3 years, 60% of individuals had an RDCI score ≥1 (versus 48% controls, p=0.003). Table 1 shows the incidences of selected comorbidities over 3 years. All analgesics were statistically significantly prescribed more in patients with a musculoskeletal disease versus controls (table 2).
Conclusion: This study highlights the issue of multimorbidity in patients with musculoskeletal diseases, especially for individuals with RA and PSA. The high cardiovascular burden is substantial in these two populations. The high prevalence of opioids in 1/5 patients with an inflammatory rheumatic disease is to be noted.
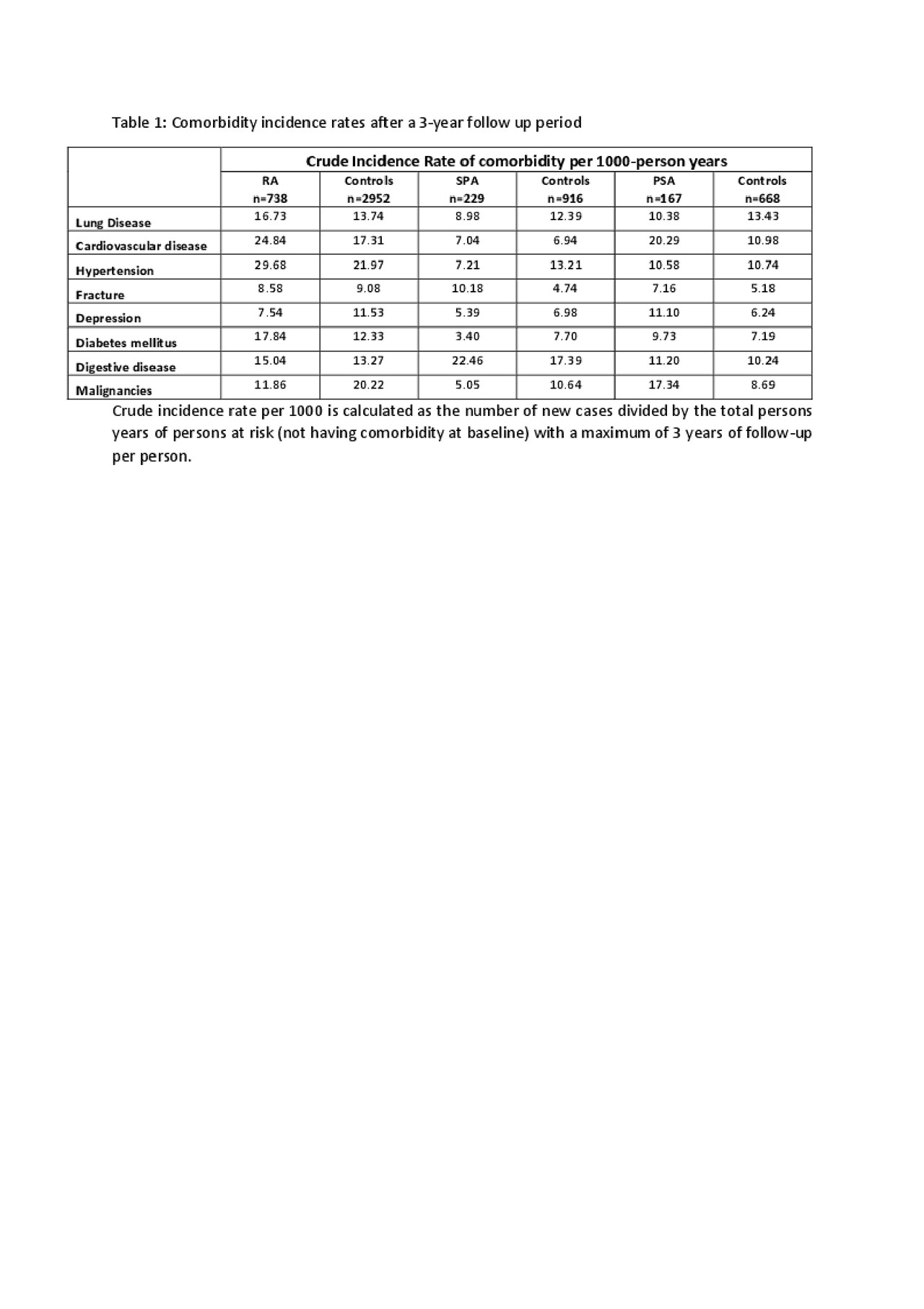
Abstract_ACR_draft3_20190604_table1
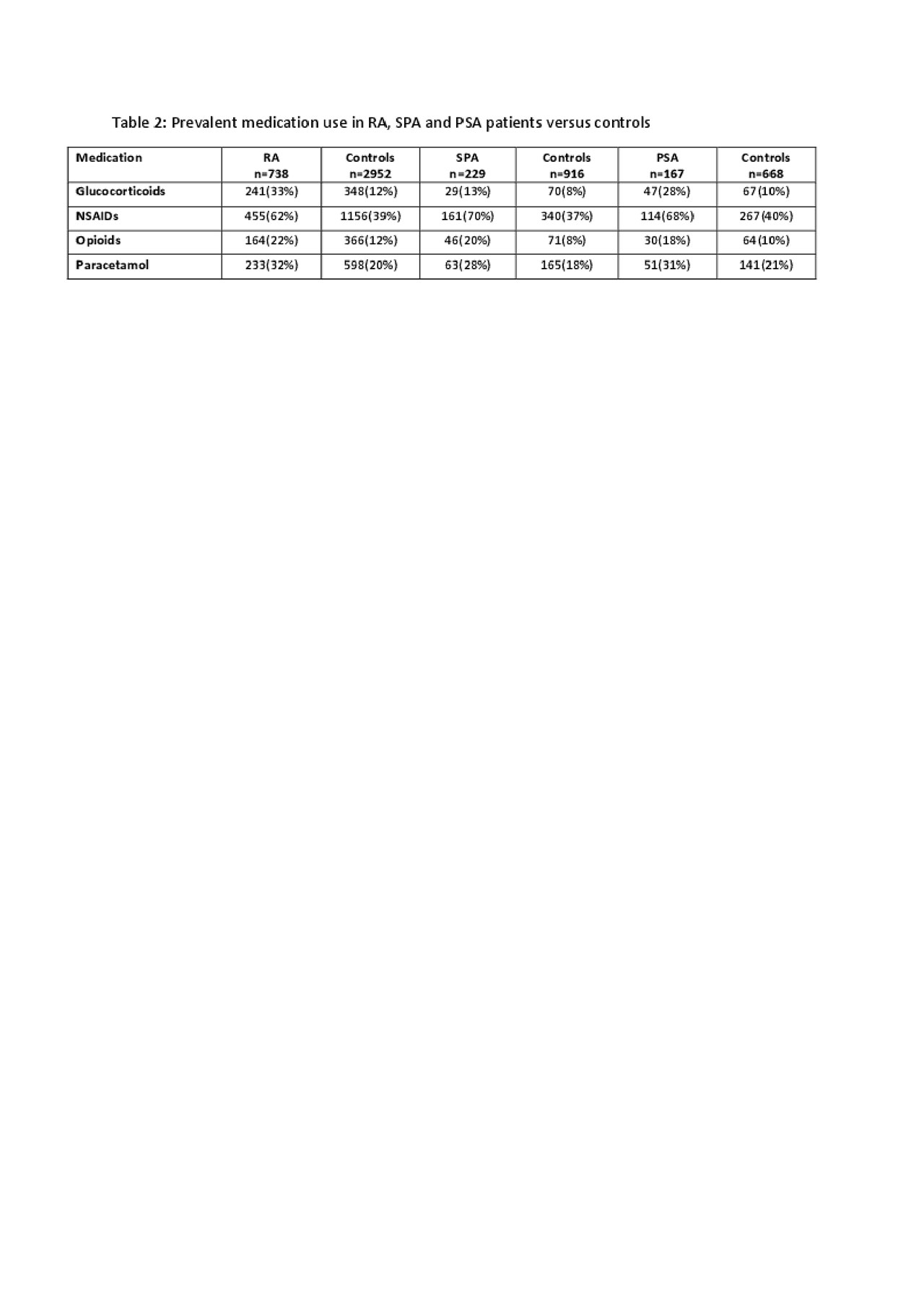
Abstract_ACR_draft3_20190604_table2
To cite this abstract in AMA style:
Pazmino S, Stouten V, Verschueren P, Mamouris P, Westhovens R, De Vlam K, Bertrand D, Van der Elst K, Vaes B, De Cock D. The Burden of Comorbidity in Patients with RA, PSA or SPA in a General Practice Registry [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/the-burden-of-comorbidity-in-patients-with-ra-psa-or-spa-in-a-general-practice-registry/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-burden-of-comorbidity-in-patients-with-ra-psa-or-spa-in-a-general-practice-registry/
