Session Information
Date: Saturday, November 6, 2021
Title: Epidemiology & Public Health Poster I: COVID-19 & Vaccination (0084–0117)
Session Type: Poster Session A
Session Time: 8:30AM-10:30AM
Background/Purpose: We previously showed that perceived stress during the COVID-19 pandemic was associated with concomitant increases in symptoms of depression and anxiety. In lupus alone, perceived stress during the pandemic was associated with concomitant increases in patient-reported disease activity, pain, fatigue, and cognitive functioning. We examined the role of both general and COVID-specific stress during the early stages of the pandemic with subsequent changes in patient-reported outcomes and comorbidities among individuals with rheumatic disease
Methods: Data are from FORWARD, The National Databank for Rheumatic Diseases, a longitudinal registry of individuals with rheumatic diseases. Data are regularly collected via semi-annual questionnaires. Participants with active emails were asked to respond to 5 COVID-19-specific questionnaires from March 25 through June 2, 2020. The COVID-19 questionnaire included an item about COVID-19-specific stress and the 4-item Perceived Stress Scale (PSS), which assesses general stress. Both stress scale scores were transformed to 0 – 10 scores to facilitate comparison. PROs examined were Patient Activity Score (PAS)-II, Health Assessment Questionnaire (HAQ)-II, and numeric rating scales for pain, fatigue, and sleep disturbance (0=no problem, 10=severe). Comorbidity burden was measured with the Rheumatic Disease Comorbidity Index (RDCI). Participant characteristics and baseline PRO scores were taken from the most recent pre-COVID-19 semi-annual questionnaire. Follow-up PRO scores were from the semi-annual questionnaire collected between July-December 2020. Predictors of PRO/RDCI worsening among respondents with rheumatoid arthritis (RA), osteoarthritis (OA), and lupus (SLE) were identified using multiple logistic regression, focusing on the role of COVID-19-specific stress and PSS, and controlling for age, sex, race, education, rural residence, disease duration, pre-COVID-19 global disease severity rating, and the pre-COVID PRO/RDCI outcome value.
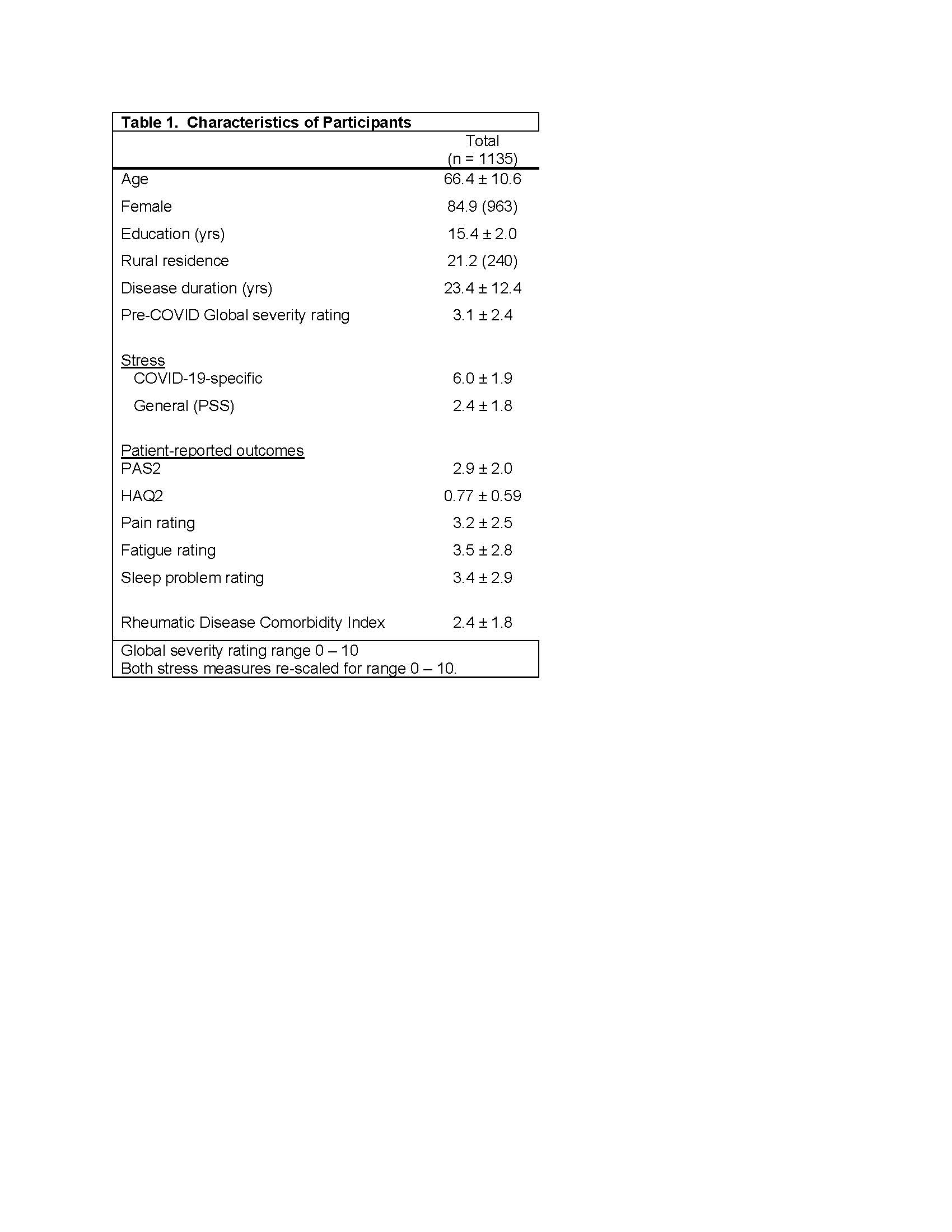
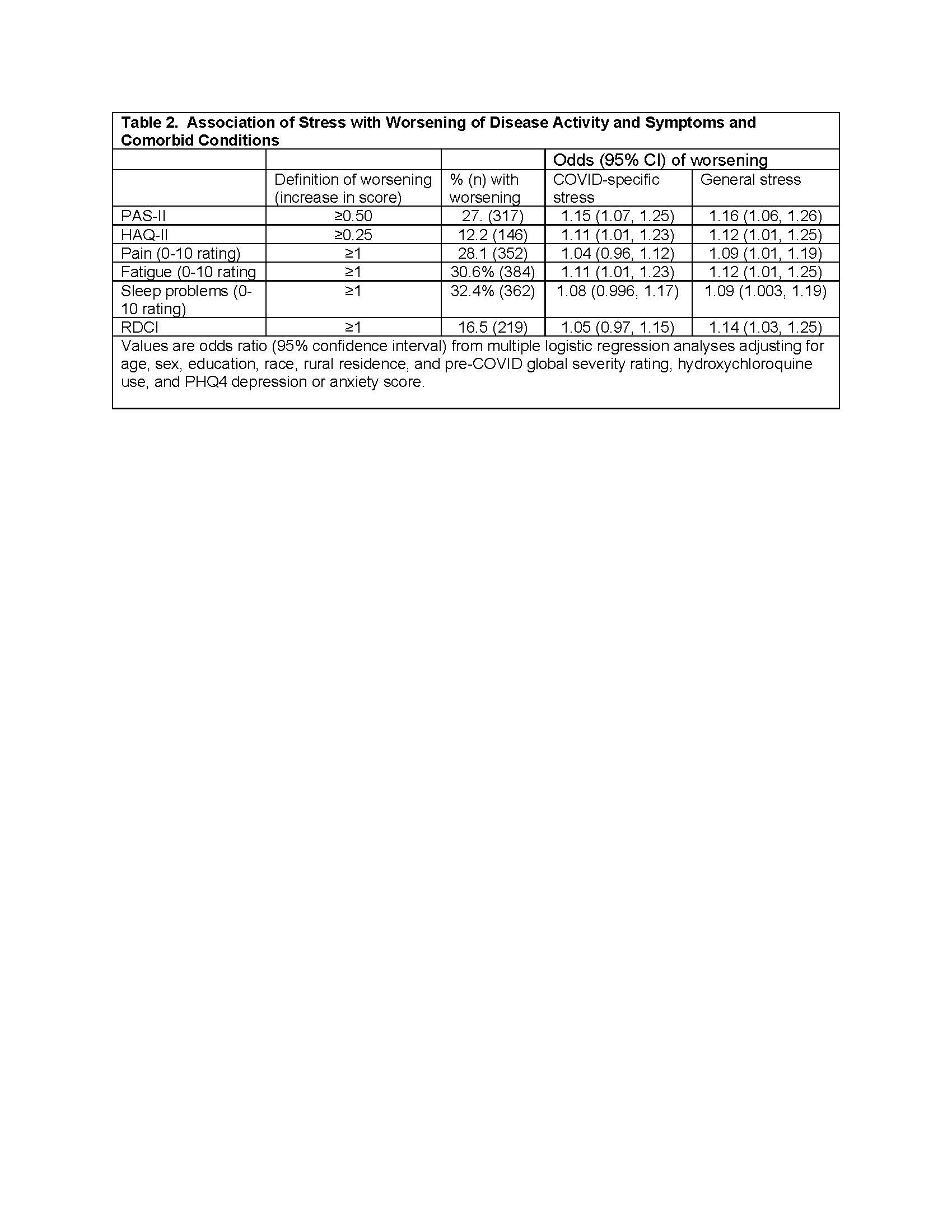
Results: 7217 participants were invited for the COVID-19 questionnaire; 2000 (28%) responded. Of these, 1135 also responded to the July 2020 questionnaire and are included in analyses (Table 1). The frequency worsening of PROs ranged from 12.2% for the HAQ2 to 32.4% for sleep disturbance (Table 2). 16.5% had an increase in RDCI. General stress during the pandemic was associated with significantly greater odds of subsequent worsening of all PROs and an increase in RDCI (Table 2). COVID-specific stress was associated with significantly greater odds of subsequent worsening of PAS2, HAQ2, and fatigue.
Conclusion: Substantial portions of these individuals with rheumatic diseases experienced worsening in patient-reported outcomes and comorbid conditions. General stress levels early in the pandemic were significantly associated with those subsequent changes. Results suggest an important role for stress levels in patient outcomes and highlight the importance of the assessment of stress in clinical settings and identification of effective stress management techniques.
To cite this abstract in AMA style:
Katz P, Wipfler K, Pedro S, Michaud K. The Association of General and Covid-19-Specific Stress with Changes in Patient-Reported Outcomes and Comorbidities [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/the-association-of-general-and-covid-19-specific-stress-with-changes-in-patient-reported-outcomes-and-comorbidities/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-association-of-general-and-covid-19-specific-stress-with-changes-in-patient-reported-outcomes-and-comorbidities/