Session Information
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Intra-articular (IA) deposition of calcium crystals (chondrocalcinosis), is common in knee OA. While calcium crystals can cause inflammatory arthritis, their contribution to joint inflammation in OA, as manifested by effusion-synovitis and Hoffa’s synovitis on MRI, is unclear. Clarifying the role of calcium crystal deposition in joint-level inflammation would provide improved understanding for the role of targeted cytokine therapy in those with IA mineralization. Prior studies have been limited by use of radiographs to detect chondrocalcinosis. In contrast, CT provides higher sensitivity for detecting IA mineralization as well as identifying potential tissue-specific effects of IA mineralization in OA. We aimed to evaluate the cross-sectional and longitudinal relation of CT-detected IA mineralization to effusion-synovitis and/or Hoffa’s synovitis on MRI with the hypothesis that IA mineralization contributes to the worsening of synovitis in OA.
Methods: We included participants from the Multicenter Osteoarthritis (MOST) Study who had knee radiographs, CTs, and MRIs. IA mineralization was assessed on CT at baseline using the Boston University Calcium Knee Score (BUCKS), a semi-quantitative 0-3 scoring of the extent of mineralization in Whole Organ MRI Score (WORMS) subregions. We categorized presence of mineralization as a BUCKS score >0 as follows: 1) anywhere in the knee (including cartilage, meniscus, joint capsule, ligaments); 2) cartilage; 3) meniscus. Effusion-synovitis and Hoffa’s synovitis were scored on MRI in one knee using MOAKS at baseline and two years later. For cross-sectional analyses, either effusion-synovitis and/or Hoffa’s synovitis were considered present with MOAKS ≥1 in either score. For longitudinal analyses, worsening was defined as an increase of ≥1 in MOAKS, for either effusion-synovitis and/or Hoffa’s synovitis scores. We evaluated the relation of IA mineralization to the presence of effusion-synovitis and/or Hoffa’s synovitis cross-sectionally and their worsening longitudinally, using binomial regression with generalized estimating equations. Analyses were adjusted for age, sex, and body mass index.
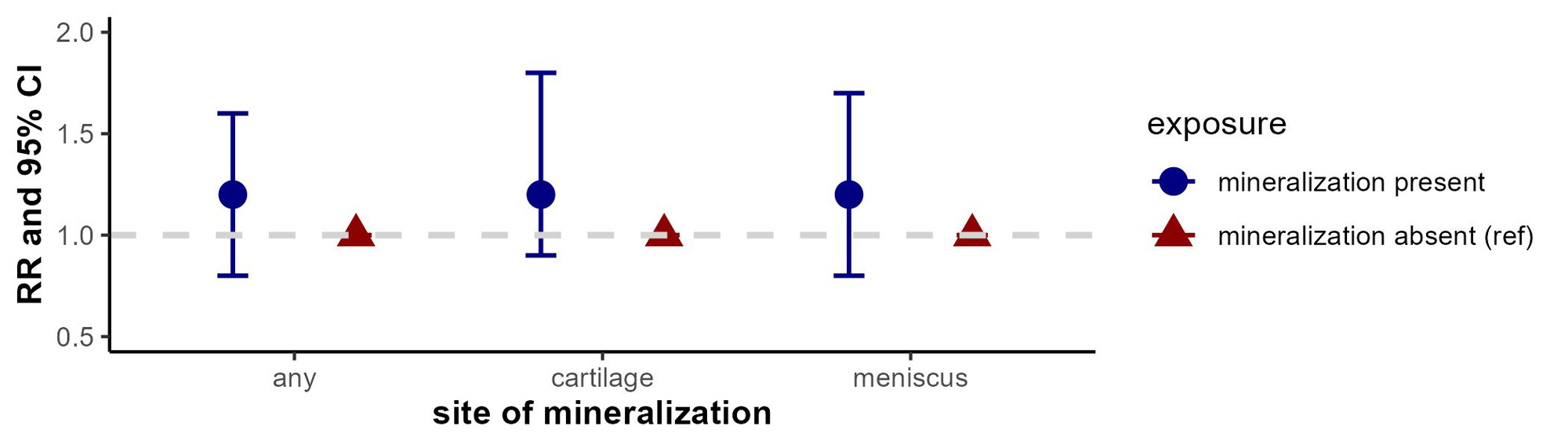
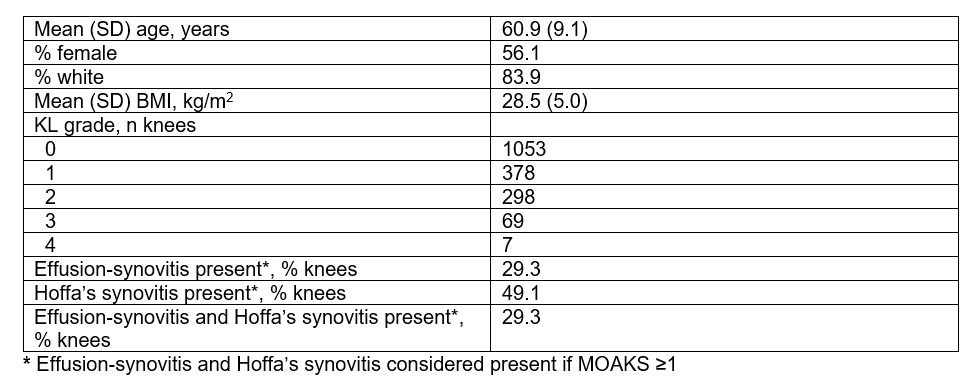
Results: We included 1668 participants (mean age 60±9, 56% female, mean BMI 28.5±5 kg/m2; 21% knees with radiographic OA) (Table). Any IA mineralization was present in 9.2%, effusion-synovitis in 49.1%, Hoffa’s synovitis in 29.3%. Overall, 16.7% had worsening of either effusion-synovitis and/or Hoffa’s synovitis on MRI at 2 years. The presence of any IA mineralization was associated with 30% higher prevalence of effusion-synovitis and/or Hoffa’s synovitis cross-sectionally (PR 1.3, 95% CI 1.1-1.5), and 20% higher risk of worsening longitudinally (RR 1.2, 95% CI 0.8-1.6) (Figure).
Conclusion: CT-detected IA mineralization in various tissues was modestly associated with effusion-synovitis and Hoffa’s synovitis at baseline and with worsening over 2 years. These findings are limited by the sample size.
To cite this abstract in AMA style:
Liew J, Rabasa G, Jarraya M, Guermazi A, Felson D, Lewis B, Lynch J, Nevitt M, Torner J, Neogi T. The Association of CT-Detected Intra-Articular Mineralization with MRI-Detected Effusion-Synovitis and Hoffa’s Synovitis in Knee OA: The Multicenter Osteoarthritis Study [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/the-association-of-ct-detected-intra-articular-mineralization-with-mri-detected-effusion-synovitis-and-hoffas-synovitis-in-knee-oa-the-multicenter-osteoarthritis-study/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-association-of-ct-detected-intra-articular-mineralization-with-mri-detected-effusion-synovitis-and-hoffas-synovitis-in-knee-oa-the-multicenter-osteoarthritis-study/