Session Information
Date: Monday, October 27, 2025
Title: (1467–1516) Systemic Lupus Erythematosus – Diagnosis, Manifestations, & Outcomes Poster II
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Since SLE is associated with significant morbidity and healthcare burden, estimates of SLE incidence are needed to inform research and public health initiatives, including rheumatology workforce planning. SLE incidence estimates may be affected by health care access or care-seeking behaviour (which may have been altered during COVID-19 pandemic years i.e. 2020-2022) and/or by changing environmental factors (e.g. viral triggers, climate change). Our objective is to estimate annual SLE incidence rates over time, using real-world US data.
Methods: Using the Merative™ MarketScan® Commercial (+/-Medicare Supplemental) databases, we identified adults (18+) with > 2 years of continuous enrollment and no SLE diagnoses during those 2 years between Jan. 2016-Dec. 2022. Among these, a 20% random sample was selected for analysis. Time zero was the first qualifying date for cohort entry. Incident SLE was defined by International Classification of Diseases diagnostic codes, based on ≥2 physician visits ≥8 weeks apart within two years and/or ≥1 hospitalization. Individuals were followed from time zero until the earliest of SLE diagnosis, health plan disenrollment, or end of follow-up. Annual SLE incidence rates were calculated with 95% confidence intervals (CI). We report incidence overall and stratified by sex, and female-specific rates were further stratified according to whether person-time was contributed during reproductive age (age younger than 52). We assessed age (continuous) and sex in a multivariate hazard regression predicting SLE onset, controlling for calendar year.
Results: We analyzed 4.6 million individuals followed an average of 2.8 years (standard deviation, SD 2.2); 52.6% were female, and mean age at time zero was 43.1 years (SD 14.8). During this period, 1,593 new SLE cases (89.2% female) were identified across 12.9 million person-years (12.3 events per 100,000 person-years). There was no clear difference in incidence comparing 2020-2022 (12.6 events per 100,000 person-years) versus 2016-2019 (12.2 events per 100,000 person-years). In any given calendar year, the incidence was (as expected) much greater among females than males (Table 1). Overall, women had a higher incidence during reproductive years (23.3 events per 100,000 person-years; 95% CI 21.9-24.9) versus later (16.8 events per 100,000 person-years; 95% CI 15.3-18.5). In multivariate models, hazard ratios (HR) for female sex was 7.47 (95% CI 6.38-8.75) and for age (continuous),1.00 (95% CI 1.00, 1.01).
Conclusion: These clinically relevant real-world data suggest SLE incidence in the US is holding steady, during the period 2016-2022. Potential limitations of our analyses include selection bias (all individuals had private insurance), short average follow-up time period, and possible outcome misclassification, including the possibility that some prevalent SLE cases were mis-characterized as incident. Additional/ongoing analyses will consider other important factors, such as urban-versus-rural residence, race/ethnicity, and environmental exposures over a longer time period.
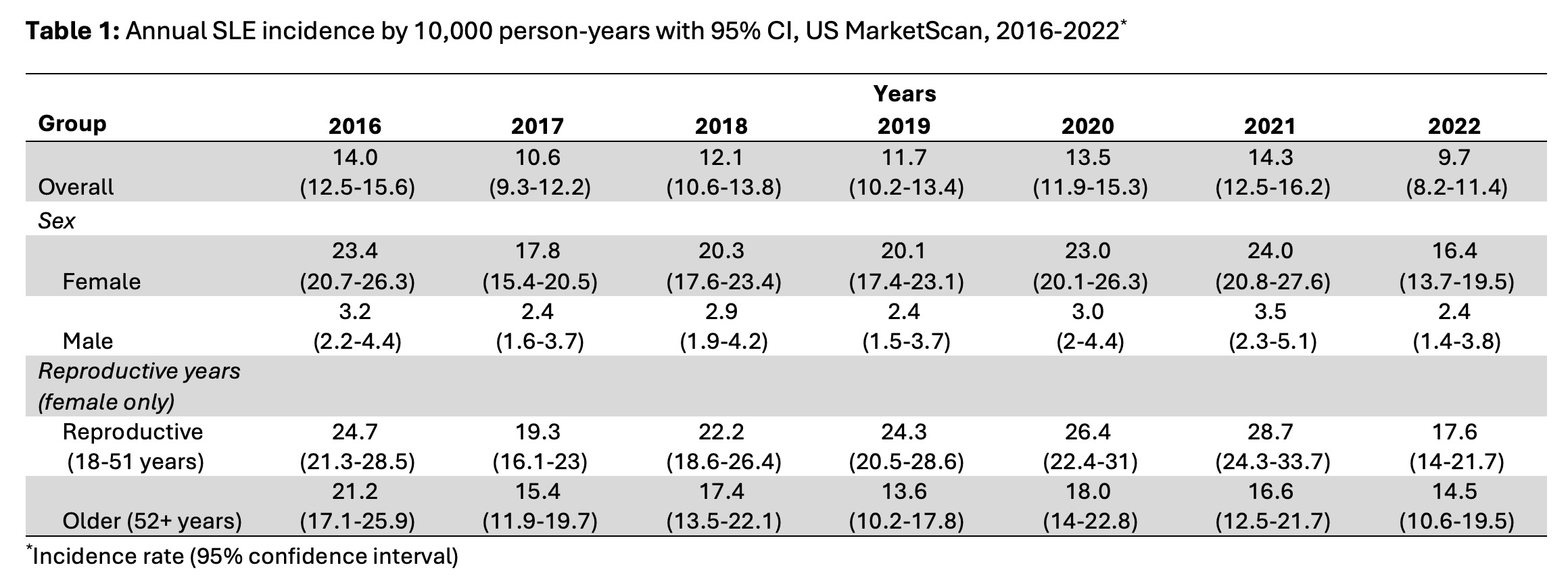 Table 1: Annual SLE incidence by 10,000 person-years with 95% CI, US MarketScan, 2016-2022*
Table 1: Annual SLE incidence by 10,000 person-years with 95% CI, US MarketScan, 2016-2022*
To cite this abstract in AMA style:
Bernatsky S, Dowell S, Banbury B, Curtis J, Wright G, Holladay E, Mudano A, Moura C, Kerr G. Temporal Trends in the Incidence of Systemic Lupus Erythematosus (SLE) in the United States (US): Holding Steady? [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/temporal-trends-in-the-incidence-of-systemic-lupus-erythematosus-sle-in-the-united-states-us-holding-steady/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/temporal-trends-in-the-incidence-of-systemic-lupus-erythematosus-sle-in-the-united-states-us-holding-steady/
