Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: There is a paucity of knowledge regarding the benefits and limitations of telemedicine in patients with SLE, particularly in those with under-resourced backgrounds. We aimed to assess the experiences and views on telemedicine of both people with SLE and their health care team members in a safety net setting.
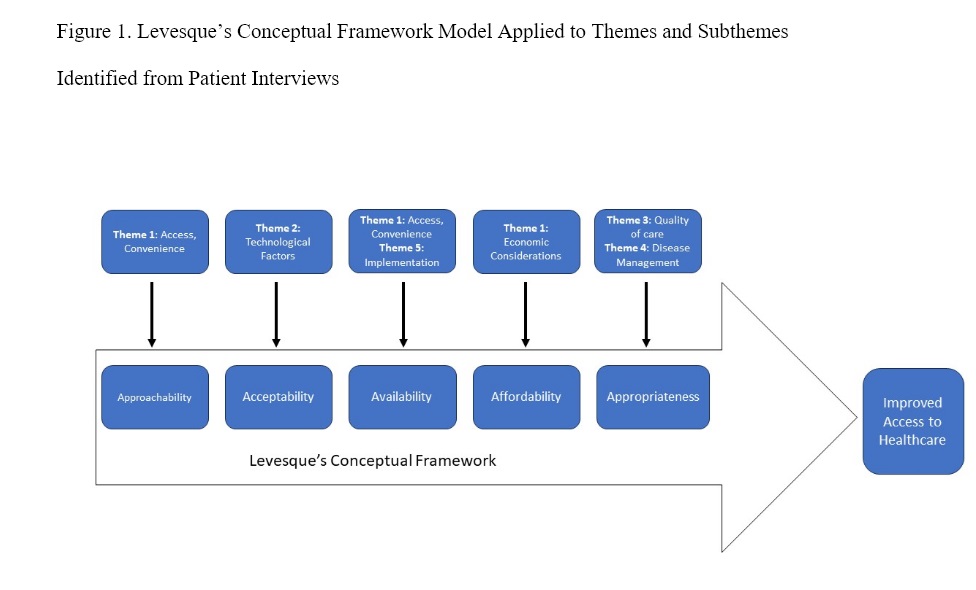
Methods: We conducted semi-structured in-person interviews of patients in a publicly-funded clinic in Harris County, Texas with SLE and health care professionals including Rheumatologists, nurses, medical assistants, and a fellow. Interviews were transcribed and then coded using inductive and deductive approaches. Data collected proceeded until thematic saturation was reached. Themes and subthemes were identified and visualized using Levesque’s Conceptual Framework for improving access to healthcare.
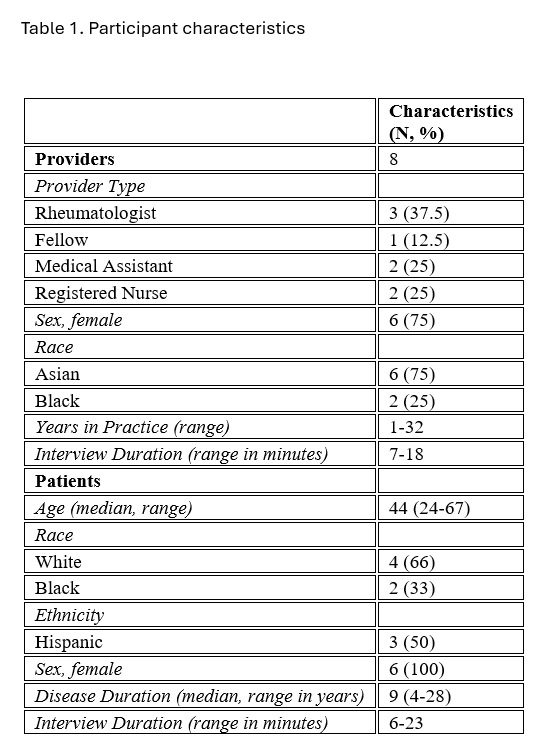
Results: Fourteen interviews were conducted. Participants included eight health care professionals and six patients with SLE (Table 1), all of whom had previously participated in telemedicine visits. Five themes were considered as major domains, including: 1) Access, Convenience, and Economic Considerations, 2) Technological factors, 3) Quality of Care, 4) Disease Management and Outcomes, and 5) Implementation of Telemedicine (Figure 1). Patients and professionals generally perceived telemedicine as a means to improve access to care and enhance convenience for patients, particularly those with transportation difficulties and physical disabilities. While telemedicine was viewed as having many potential benefits, there was concern amongst both patients and providers about digital literacy and access to technology. The perceived impact of telemedicine on the quality of care in patients with SLE varied amongst participants. Rheumatologists and nurses expressed concern about its negative impact on the physician-patient relationship and the limited ability to conduct physical examinations. Health care professionals also generally perceived telemedicine to be appropriate for stable patients with low disease activity. However, the suitability of telemedicine for SLE flares varied amongst participants. Rheumatologists generally felt disease flares were better managed through in-person visits, whereas some patients and nurses perceived telemedicine to be beneficial for flares because of quicker access to a clinician. Both patients and health care professionals made recommendations to facilitate implementation of telemedicine including providing patients with adequate training on telemedicine platforms either through tutorials or in person training, ensuring access to adequate technology, and establishing protocols and technical support during virtual visits.
Conclusion: In this qualitative study, barriers to telemedicine including digital literacy, possible impact on physician-patient relationship, and language barriers, were identified. By addressing these challenges and leveraging the benefits of telemedicine, we have the opportunity to improve access to care in patients with SLE, particularly from under-resourced backgrounds.
To cite this abstract in AMA style:
Bruera S, Bowman S, Ferguson K, Maliekel M, Lopez-Olivo M, Suarez-Almazor M, Danila M, Yazdany J, Agarwal S. Telemedicine for Under-resourced Patients with Systemic Lupus Erythematosus: A Qualitative Study Exploring the Views and Experiences of Patients and Rheumatology Health Care Professionals [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/telemedicine-for-under-resourced-patients-with-systemic-lupus-erythematosus-a-qualitative-study-exploring-the-views-and-experiences-of-patients-and-rheumatology-health-care-professionals/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/telemedicine-for-under-resourced-patients-with-systemic-lupus-erythematosus-a-qualitative-study-exploring-the-views-and-experiences-of-patients-and-rheumatology-health-care-professionals/