Session Information
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Rheumatic diseases are associated with accelerated atherosclerosis, and an increase in cardiovascular morbidity and mortality. This process is mediated by classic cardiovascular risk factors (CVRF), chronic inflammation and atherogenic treatments such as corticosteroids. In Systemic Sclerosis (SSc) cardiovascular complications have increased in recent decades, although the studies on subclinical atherosclerosis (sATS) in SSc show discordant results. Our objetive is to evaluate prospectively the relationship between subclinical atherosclerosis, cardiovascular morbidity and mortality in patients with SSc.
Methods: 120 consecutive patients with SSc who attended their medical regular review during November and December 2011 were included. We evaluated the presence of plaques and measured the right CCA IMT by B doppler US for the detection of sATS (IMT > 0.9mm and/or presence of plaque), review of classic CVRF and estimation of Medsger severity and EUSTAR activity index. Patients have been followed for 8 years, with at least annual consultation. In retrospect, the SCTC damage index, published in 2019, was obtained at the time of inclusion in the study. The clinical characteristics of the patients are collected since 1990 in a Prospective Longitudinal Observational Study (PLOS). Descriptive analysis was performed, using contigence tables for qualitative variables, and comparison of means for quantitative variables. The relationship between clinical characteristics, mortality, cardiovascular events (CVE), activity, severity and damage index, and sATS, was analyzed using binary logistic regression, adjusting for age and sex.
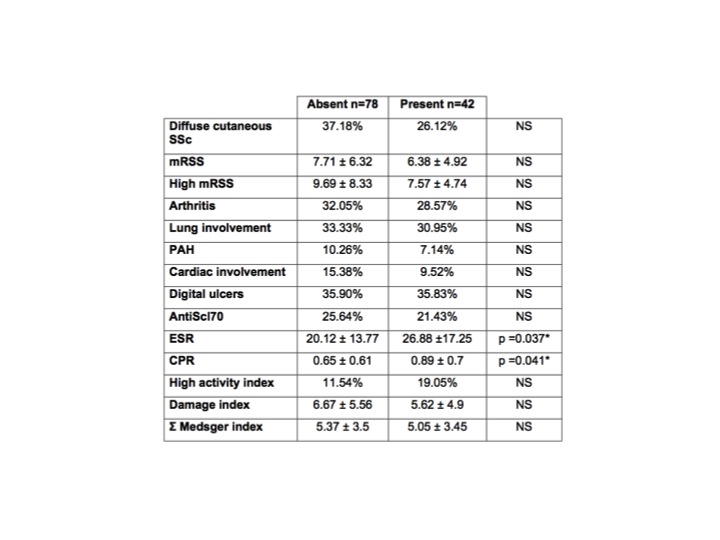
Results: 120 patients with SSc were included (93% female, age 60 ± 12 years). 42 of these patients (35%) had subclinical atherosclerosis. Age was statistically significant higher in patients with sATS compared to those without it (67.9±11.5 vs. 56.1±10.4 years, p < 0.001). We found no differences between groups in activity, damage and severity index (Table 1). Patients with sATS had higher levels of ESR and CRP, but the difference was not confirmed after adjusting for age (*). During the 8 years of follow- up, 9 CVE in 7 patients (5.8%): three myocardial infarction, one transient ischemic accident, one angor, one intermittent claudication and three refractory heart failure. The incidence of severe CVE was more than double in patients with SAtS (10.25% vs. 3.7%), but the difference was not significant. We found no relationship between the mortality of any cause, or the secondary to CVE, with sATS, in the 32 patients who died during the follow-up, 3 due to CVE (9.4%). The results are similar when we analyze only the presence of plaques.
Conclusion: In our study subclinical atherosclerosis is not related to higher mortality in patients with SSc, but it does seem to influence the occurrence of cardiovascular events. In addition, our results suggest that SSc does not influence the onset of accelerated atheromatosis.
To cite this abstract in AMA style:
Retuerto M, Rosales J, Martin M, Joven B, Carreira P. Systemic Sclerosis: Subclinical Aterosclerosis and Morbimortality [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/systemic-sclerosis-subclinical-aterosclerosis-and-morbimortality/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/systemic-sclerosis-subclinical-aterosclerosis-and-morbimortality/