Session Information
Session Type: Poster Session (Monday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Interstitial lung disease (ILD) is frequent manifestation and a leading cause of mortality in systemic sclerosis (SSc). Some SSc-related autoantibodies (aAbs), especially anti-topoisomerase I (ATA), are associated with an increased prevalence of ILD. In contrast, anti-centromere (ACA) may be protective. The association with other aAbs is unclear and it is unknown whether aAb profiles can predict the rate of ILD progression. Our goal was to examine the incidence of SSc-ILD and its subsequent progression between different aAb profiles. We hypothesized that while aAbs predict ILD development, all SSc-ILD progress similarly.
Methods: SSc subjects without pre-existing ILD in a large multi-center longitudinal cohort from 2004-2018 were included. ILD was defined by the presence of high-resolution computed tomography (HRCT) findings, or if no HRCT was available, then either a chest x-ray showing interstitial fibrosis, and/or the presence of “velcro like crackles” on exam. Clinically meaningful progression of ILD was defined using OMERACT criteria(1) of ≥10% relative decline in FVC, or ≥5% to < 10% relative decline in FVC and ≥15% relative decline in DLCO. Subjects were grouped based on single specificity aAbs: ATA, ACA, anti-RNA polymerase III (ARA), anti-PM/Scl, anti-Ku, anti-Th/To (hPOP1), anti-fibrillarin (AFA), or negative aAbs. The time to ILD onset was compared between groups using Kaplan Meier and multivariate Cox analyses adjusted for age, gender, diffuse (vs. limited) subset, physician global assessment of severity, immunosuppression exposure at or prior to baseline and presence of anti-Ro52/TRIM21 antibodies. In those with incident ILD, the time to clinically meaningful progression and mortality after ILD onset were examined. ATA served as the reference for all comparisons.
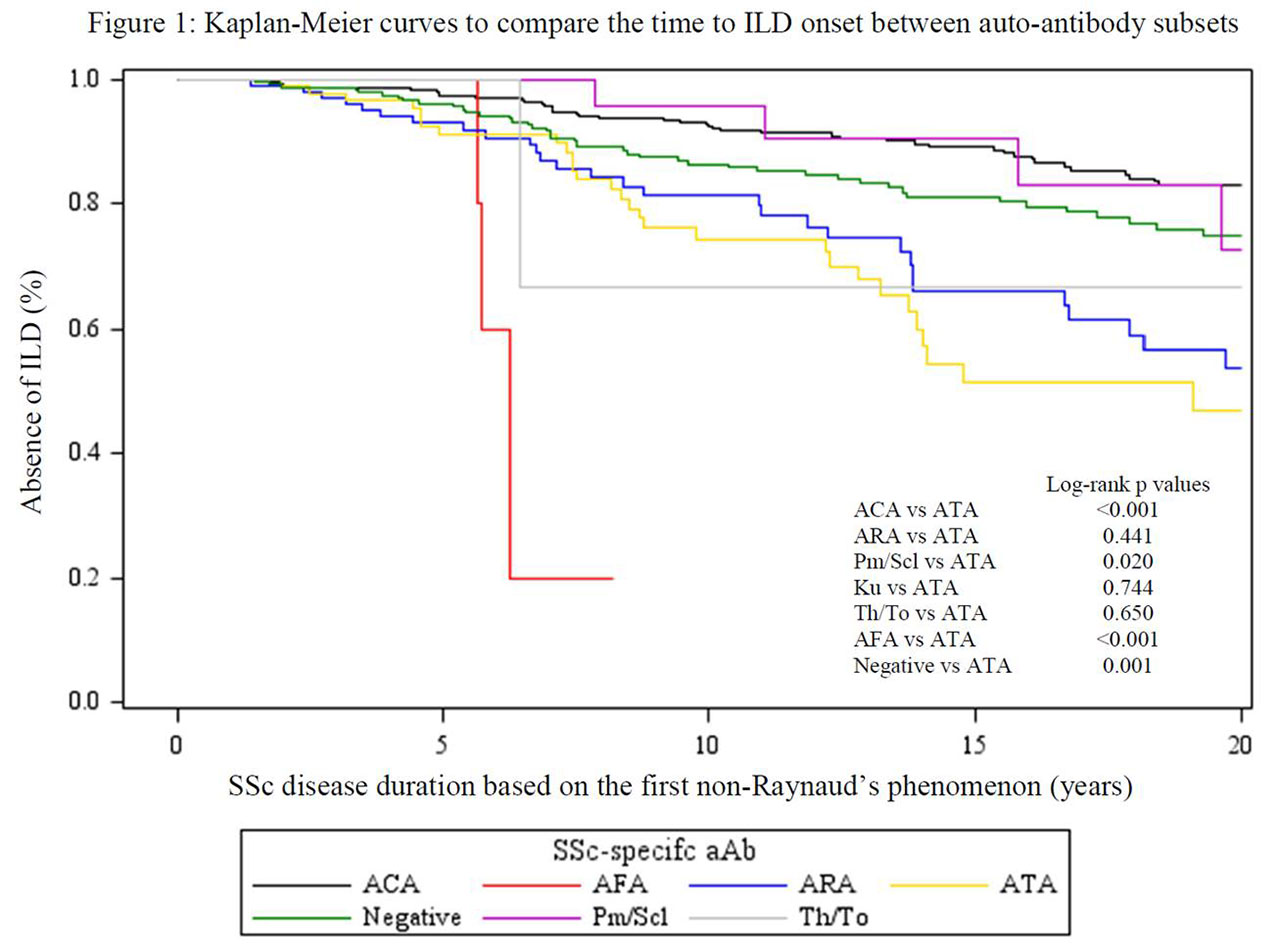
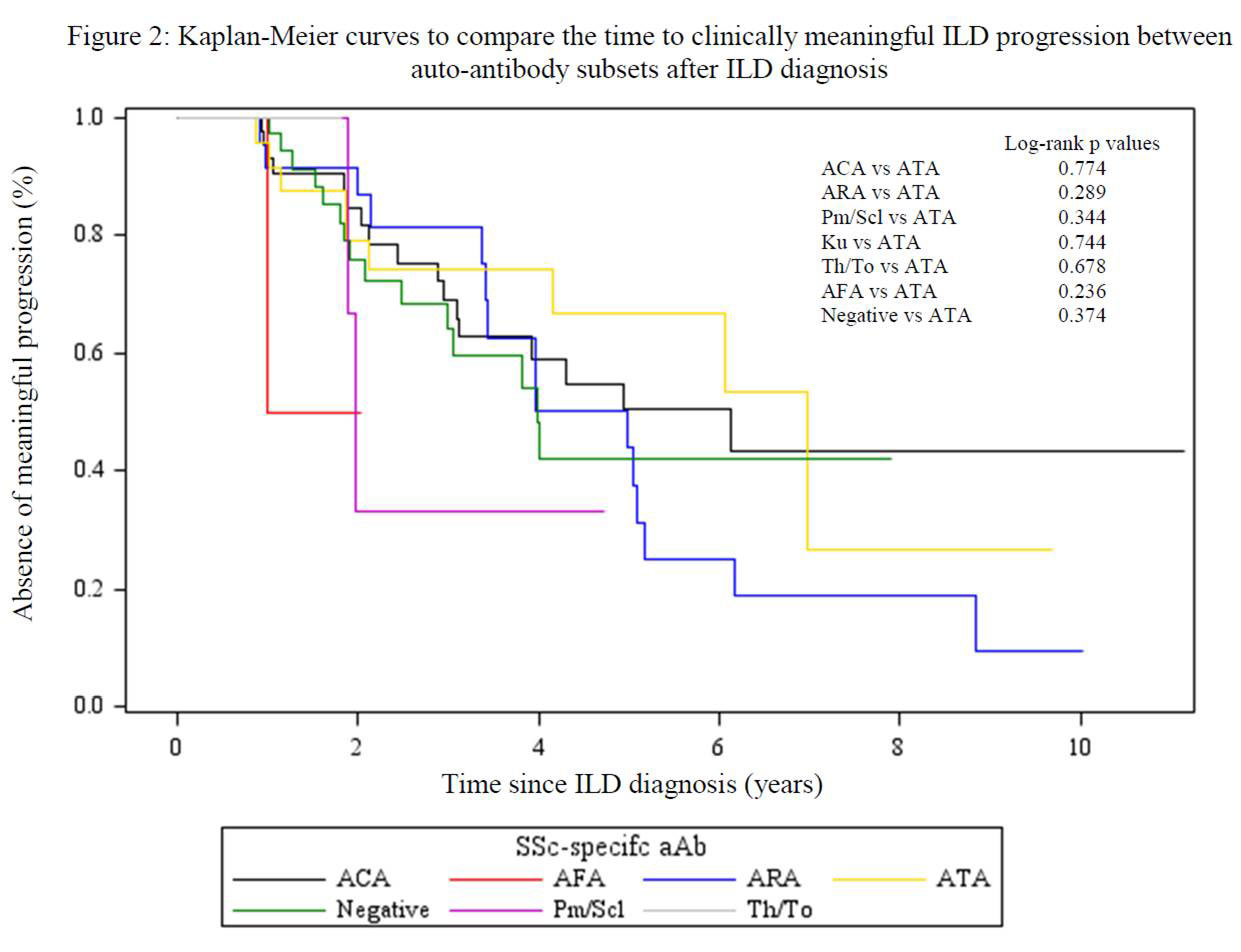
Results: Of 931 patients, 190 (20%) developed ILD: 60/429 (14%) ACA, 31/94 (33%) ATA, 32/114 (28%) ARA, 6/24 (25%) anti-Pm/Scl, 0/2 anti-Ku, 2/5 (40%) anti-Th/To, 4/5 (80%) AFA, and 55/258 (21%) negative aAb. Subjects with ATA developed ILD earlier than ACA, anti-PM/Scl and negative aAb groups (log rank p < 0.01, p = 0.02 and p < 0.01, respectively), although AFA group had the most rapid onset (p < 0.01) (Figure 1). In multivariate analyses, ACA and negative aAb groups were less likely (HR (95% CI) 0.36 (0.22, 0.57) and 0.53 (0.34, 0.84) respectively), whereas AFA was more likely (HR (95% CI) 4.12 (1.22, 13.86)) to develop ILD compared to ATA. On the other hand, no differences in the time to clinically meaningful ILD progression (Figure 2) or survival after ILD onset were found between groups.
Conclusion: Compared to patients with ATA, AFA conferred a higher risk of developing ILD, whereas ACA, anti-PM/Scl and the absence of SSc specific aAbs were associated with a lower risk. Nevertheless, ILD developed in all aAb sub-groups and, once present, the aAb profile was not associated with ILD progression or subsequent mortality.
- Khanna D, Mittoo S, Aggarwal R, Proudman SM, Dalbeth N, Matteson EL, et al. Connective Tissue Disease-associated Interstitial Lung Diseases (CTD-ILD) – Report from OMERACT CTD-ILD Working Group. The Journal of rheumatology. 2015;42(11):2168-71.
To cite this abstract in AMA style:
Zheng B, Wang M, Fritzler M, Choi M, Baron M, Hudson M. Systemic Sclerosis Auto-antibody Profiles Predict Interstitial Lung Disease Onset but Not Progression [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/systemic-sclerosis-auto-antibody-profiles-predict-interstitial-lung-disease-onset-but-not-progression/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/systemic-sclerosis-auto-antibody-profiles-predict-interstitial-lung-disease-onset-but-not-progression/