Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Systemic juvenile idiopathic arthritis (sJIA) is a chronic disease that results in significant morbidity and mortality in children1. Improved understanding of the pathophysiology of sJIA has led to recent therapeutic advances including a growing evidence base for the earlier use of IL-1 or IL-6 blockade2. We aim to describe our experience of sJIA over a period of 15 years which includes clinical presentation, therapeutic interventions and the heterogeneity around the use of biologics spanning over this period, and the clinical outcomes at different time points over the course of the disease.
Methods: Children with a diagnosis of sJIA treated at Bristol Royal Hospital for children from 2010 to 2025 were included. Electronic medical records were reviewed retrospectively. Details regarding patient demographics, clinical features, laboratory parameters, treatment and outcomes were recorded. Patients were categorized as monocyclic, polycyclic and persistent depending on the disease course. Data was analyzed using descriptive statistics.
Results: A total of 80 children diagnosed with sJIA-29 (36.25%) monocyclic, 12(15%) polycyclic, 39(48.75%) were persistent. The mean age of diagnosis 7.6 (0.8-16) years. 43(53.75%) were females. Apart from fever (in 100%), other common presentations included rash 67(83.8%), arthritis 54(67.5%), splenomegaly 23(28.8%). Median(IQR) laboratory investigations at diagnosis included haemoglobin 98gm/L(85-112), white cell count 18*109(10-26), platelets 411 *109(288-549), C-reactive protein 121mg/L(63-195), ESR 75mm/hr(25-136),D-dimer 3089ng/mL(1359-6106), LDH 501U/L(345-902), fibrinogen 5.2ng/mL(3.4-6.4), ferritin 1443mcg/L(459-4415), triglycerides 1.5mmol/L(1-2.3), ALT 26 U/L(12-65). Treatment received primarily was variable over the 15 year span and included combination of corticosteroids, disease modifying anti-rheumatic drug, IL-1 and IL-6 blockade. IL-1/IL-6 blocker therapy initiated in 15(18.8%) within 3 months of diagnosis and 39(48.7%) by the end of 1 year. Maximum disease inactivity off treatment was achieved in the monocyclic group(80.8%). Disease activity controlled on treatment was achieved in 62.5% in polycyclic and 56.4% in persistent group. At the end of 5 years, 5/8 in polycyclic and 6/30 in persistent achieved clinical remission off treatment.
Conclusion: sJIA is a disease with the variable course that determines the outcome. Based on our study, it has been observed that children in persistent category required combination of therapies to keep the disease under control.1Singh-Grewal D, Schneider R, Bayer N, Feldman BM. Predictors of disease course and remission in systemic juvenile idiopathic arthritis: significance of early clinical and laboratory features. Arthritis Rheum. 2006 May;54(5):1595–601.2Foley CM, McKenna D, Gallagher K, McLellan K, Alkhdher H, Lacassagne S, et al. Systemic juvenile idiopathic arthritis: The Great Ormond Street Hospital experience (2005-2021). Front Pediatr. 2023;11:1218312.
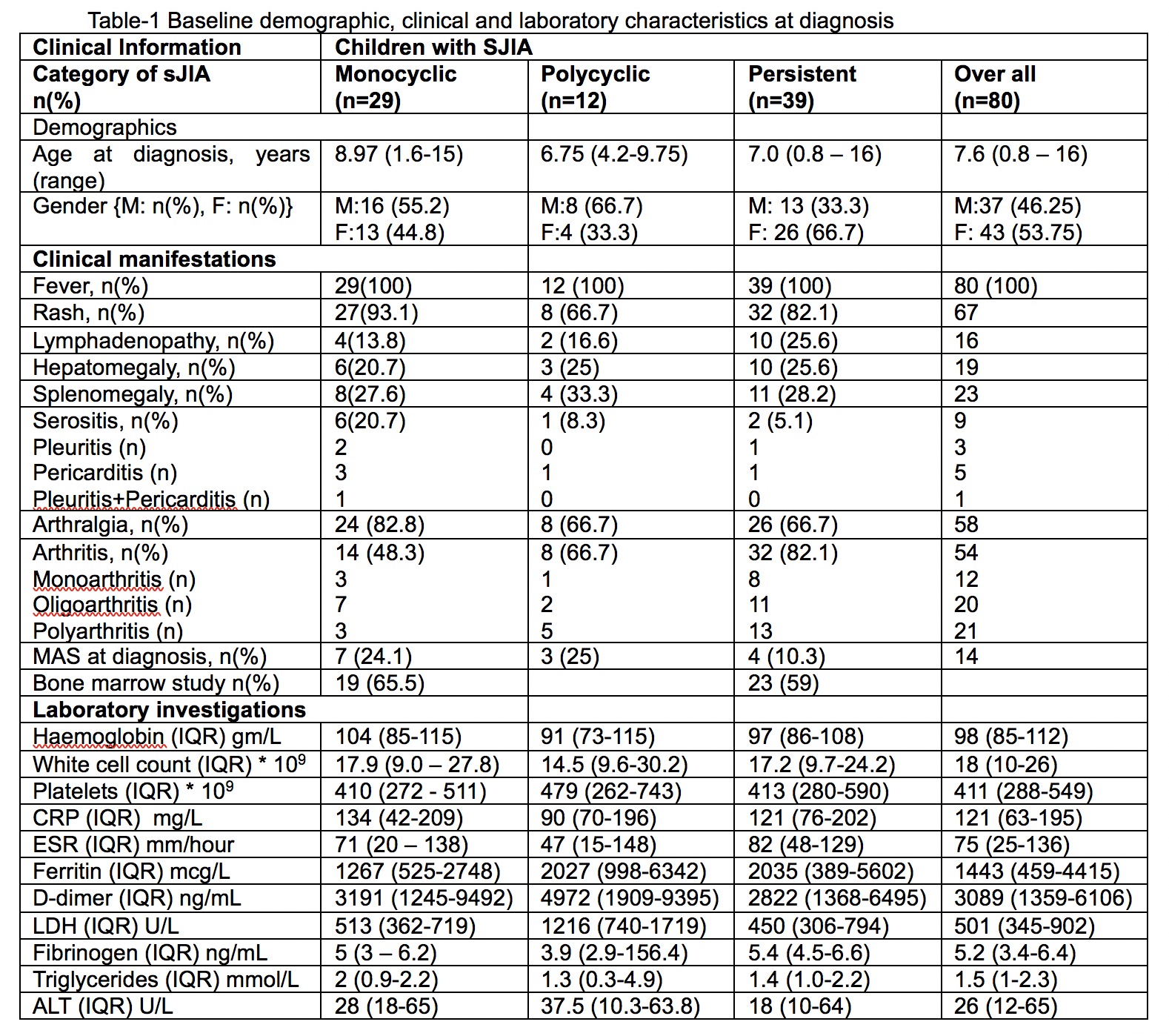 Table-1 Baseline demographic, clinical and laboratory characteristics at diagnosis
Table-1 Baseline demographic, clinical and laboratory characteristics at diagnosis
.jpg) Table 2: Treatment received during the disease course
Table 2: Treatment received during the disease course
.jpg) Disease outcome following treatment
Disease outcome following treatment
To cite this abstract in AMA style:
Batchu Prithvi A, Govardhan C, Aladaileh B, V Ramanan A. Systemic juvenile idiopathic arthritis- Fifteen-year experience from a tertiary centre at Bristol, United Kingdom [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/systemic-juvenile-idiopathic-arthritis-fifteen-year-experience-from-a-tertiary-centre-at-bristol-united-kingdom/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/systemic-juvenile-idiopathic-arthritis-fifteen-year-experience-from-a-tertiary-centre-at-bristol-united-kingdom/
